CHAPTER ONE
Pestilence and Headcolds
1
 On December 2, 1761, Doña Luisana Grande Acxotlan of Cholula was sick in bed . . .
Was there ever a time in humanity's history that did not include disease? The ancient Greeks mark the beginning of pestilence and other torments of the flesh by the fable of Pandora's box, whereas the Judeo-Christian tradition explains that disease and death became part of the human condition when Eve successfully tempted Adam into tasting the forbidden fruit. Today we know that the diseases of humanity evolved in tandem with its civilizations. Beginning roughly 11,000 years ago, various peoples began the slow process of domesticating animals and plants, ultimately setting the stage for the development of what Jared Diamond has aptly called "guns, germs, and steel." This transition from hunter-gatherers to farmers set off a long chain of events in the evolution of humanity. The cultivation of crops and herd animals allowed for surplus food production, which led to a sedentary lifestyle, a growing population in more densely packed living conditions, and non-food-producing specialists. These specialists, in turn, evolved into roles we now associate with civilized societies: political elites, bureaucrats, priests, artisans, and scribes. Travel, trade, and warfare, all impossible without domesticated animals serving as land transport and carriers of goods, soon followed, intermingling humans as never before. Infectious diseases arose right alongside this sequence of civilizing advancements. Those farmers and herdsmen who were the first to raise large quantities of crops and animals also unintentionally produced large numbers of human predators: rats, roaches, houseflies, mosquitoes, worms, fungi, and bacteria. The resulting "diseases of civilization"—smallpox, measles, typhus, and the flu—began, researchers now tell us, in the close physical relationship the Old World's peoples had with their herds of cattle, sheep, goats, horses, and pigs. Thus, the real origins of humanity's diseases are found in its greatest achievements.1
On December 2, 1761, Doña Luisana Grande Acxotlan of Cholula was sick in bed . . .
Was there ever a time in humanity's history that did not include disease? The ancient Greeks mark the beginning of pestilence and other torments of the flesh by the fable of Pandora's box, whereas the Judeo-Christian tradition explains that disease and death became part of the human condition when Eve successfully tempted Adam into tasting the forbidden fruit. Today we know that the diseases of humanity evolved in tandem with its civilizations. Beginning roughly 11,000 years ago, various peoples began the slow process of domesticating animals and plants, ultimately setting the stage for the development of what Jared Diamond has aptly called "guns, germs, and steel." This transition from hunter-gatherers to farmers set off a long chain of events in the evolution of humanity. The cultivation of crops and herd animals allowed for surplus food production, which led to a sedentary lifestyle, a growing population in more densely packed living conditions, and non-food-producing specialists. These specialists, in turn, evolved into roles we now associate with civilized societies: political elites, bureaucrats, priests, artisans, and scribes. Travel, trade, and warfare, all impossible without domesticated animals serving as land transport and carriers of goods, soon followed, intermingling humans as never before. Infectious diseases arose right alongside this sequence of civilizing advancements. Those farmers and herdsmen who were the first to raise large quantities of crops and animals also unintentionally produced large numbers of human predators: rats, roaches, houseflies, mosquitoes, worms, fungi, and bacteria. The resulting "diseases of civilization"—smallpox, measles, typhus, and the flu—began, researchers now tell us, in the close physical relationship the Old World's peoples had with their herds of cattle, sheep, goats, horses, and pigs. Thus, the real origins of humanity's diseases are found in its greatest achievements.1
2As everyone now knows, these pathogens eventually played a critical role in the conquests of the New World, whose inhabitants had no immunity to the Old World diseases brought by the conquistadors and early settlers. This virulent and, from the point of view of the sufferers, incomprehensible onslaught of disease marks a decisive moment in Mexico's history. It also forms the most dramatic part of our story about the connections between the quest for health and everyday life in New Spain. But even in times when pestilence was subdued, ordinary illnesses and bodily discomforts were daily preoccupations for all groups of society. With this chapter, we begin our look at the circumstances surrounding health by identifying and describing—in the sufferers' own words whenever possible—the maladies that afflicted Mexicans before the arrival of modern medicine. We begin with Mesoamerica, where recent scholarship has uncovered new clues about the overall health of ancient Mexicans. The rest of this chapter explores the health problems of the inhabitants of New Spain, beginning with the frequent outbreaks of pestilence and other infectious diseases, on through to the more common ailments of everyday life.
^topAncient Mesoamerica
3In sharp contrast to the images of death and destruction initiated by the European conquest, precontact American populations have often been depicted by popular, and some scholarly, interpretations, in almost utopian terms. Lately, this image of strong, vigorous, and healthy populations living in a pre-Columbian paradise is being challenged by scholars examining the skeletal evidence of early settlements. Recent paleodemographic studies are revealing Mesoamericans as having been more similar to their Old World contemporaries than previously thought. Short, hard lives plagued by poor nutrition and ill health were the rule for most ordinary people. Although the pre-Columbian populations may not have suffered from the waves of epidemics that killed so many people in Old World cities, the evidence shows that physiological stress in the form of infection and undernutrition was common, if not chronic, in many ancient Mesoamerican urban settlements. Calculations of life expectancy point to short lives: at birth, life expectancy was only 15–20 years; if one made it to age 15, he or she could expect to live another 13 to 29 years, in other words, to age 28 through 44 on average. Estimates of infant mortality have been put as high as around 30 percent—40 percent. These figures show two things: that infancy was perhaps the most perilous stage in a person's life; and, this extremely high death rate of infants and children was what kept these growing populations—women averaged 8.8 births in their lifetime—in check.2
4Most historians agree that the populations of precontact America did not suffer from the "crowd-type" epidemic diseases that afflicted Old World cities, the reasons for which will be discussed later in this chapter. This does not mean, however, that there were no epidemics. Mesoamerican sources mention pestilence as one of the calamities that occurred periodically, usually during a time of prolonged famine. The Historia chichimeca tells of a "catarro pestilencial" that came during the unusually cold weather of 1454, from which many people died. For the next three years, an unremitting cycle of drought and freezing temperatures brought about a catastrophic situation for the Nahuas, as they endured the twin scourges of hunger and sickness.3 But information about the health of pre-Colombians is still too meager to even speculate on what diseases would have periodically reached epidemic levels. Their endemic diseases and health problems, however, are being made more visible by the recent work of paleopathologists.4 Skeletal remains, the primary source of evidence for these scholars, contains a considerable amount of data about the physical lives of people from all periods of Mesoamerican history. Although not as revealing as soft tissue, human bones, nonetheless, record important information about causes of death, the incidence and severity of chronic diseases, traumas from accidents or warfare, and the biomechanical patterns from habitual work. Interpretation of the skeletal record, however, is not perfect, as not all diseases affect bone and some diseases can affect bone in similar ways.5
5Many scholars have theorized a correlation between the rise of agriculture and the increased incidence of disease in ancient populations. The general notion is that as populations shifted their subsistence from foraging to agriculture their settlement pattern changed from mobility to sedentism. An increasing population density led to sanitation problems, producing ideal conditions for the spread of infectious disease. Large urban populations also entailed increasing social complexity, creating inequalities of wealth and access to basic resources.6 Temporal trends in precontact Central Mexico, with its long history as the center of Mesoamerican civilization, seem to support this hypothesis. Skeletal evidence shows a general trend of increased incidence of disease as Mesoamerica evolved from the Preclassic period (1600 BC–AD 300)—where the densest settlements were villages, where social and economic differentiation was present but not greatly elaborated, and where subsistence was based on agriculture but supplemented regularly by foraging of wild resources—to the Classic (AD 300–900) and Postclassic (900–1521) periods. In these latter epochs, more and more people came to live in densely populated cities with poor sanitary conditions, ate a more monotonous diet based on squash, corn, and beans, and experienced much greater social and economic differentiation. This change in the way people lived coincided with a trend toward a decline in the stature of Mesoamericans, from the Preclassic to the Postclassic. Shortening stature may have been an adaptive response to malnutrition, under-nutrition, and chronic infection in childhood.7 Like preindustrial cities in Europe, Mesoamerican urban settings with dense populations are believed to have had problems with public sanitation and contaminated water supplies, which help explain their high rates of infectious diseases and high mortality. Although cities in central Mexico like Teotihuacan and Tenochtitlan were situated in an arid highland environment, which would have been beneficial in curtailing the threat of some diseases spread by insects, it would have been difficult to prevent contamination of the water supply. This part of North America has a monsoonal rain pattern, where most of its rain falls from the beginning of the month of June through September, while the rest of the year receives trivial quantities of rainfall—too little to refresh nearby reservoirs. Residents of these urban areas would have drawn some of their drinking water from year-round springs, but the reservoirs and lakes surrounding the cities would have also served as a fresh water source. During the dry season, without the rains to wash away much of the human waste and trash, these bodies of waters would have been the source of many parasitic and endemic intestinal infections. The newborns and young children of these settlements would have been especially vulnerable in such an environment because an important cause of neonatal mortality is infection. Infants can become infected with such diseases as conjunctivitis, pneumonia, osteomyetitis, and meningitis, to name a few that were probably present in ancient Mesoamerica. Moreover, the bacteria that cause diarrhea are easily transmitted to babies at birth from an infected birth canal or the hands of birth attendants and parents. These diarrheal infections are the kinds of illnesses that would have run rampant in the urban settings of Mesoamerica, where inadequate disposal of human wastes and a lack of water for cleaning, especially during dry periods, would have created the perfect environment for pernicious viruses.8
6
 The Cook
Mesoamerican skeletons also reveal that a settled way of life was hard on the joints and teeth. One way in which the Old and New Worlds differed was the latter's lack of beasts of burden (except the llama, which carried light loads) and technology which aided in strenuous tasks, such as the wheel or iron tools. Mesoamerica was a society powered largely by human muscle. Human bodies were the principle mechanism for growing food, erecting buildings, and transporting heavy burdens and goods. Hard and repetitive work imposed a severe toll on the bodies of both men and women, especially on the joints required for mobility, manipulation of objects, or bearing loads.9 Skeletal evidence from the Classic and Postclassic periods tends to show a higher occurrence of degenerative joint disease than populations from earlier times, reflecting the biomechanical stress that common people might have experienced when they shifted from a hamlet-like subsistence economy to an urban one based on trade. The wear and tear on Mesoamerican joints also reflects the division of work along gender lines. Women display significantly more joint disease of the wrists than men, not surprising given that the preparation of maize tortillas, the main source of calories, was a laborious task that had to be preformed twice a day by the women of the family. Men, the carriers of heavy loads, tend to show greater mechanical stress in the neck and lumbar region.10 Life based on agriculture also took its toll on the teeth of Mesoamericans. Although the dental wear and tear caused by the consumption of foraged foods was reduced over time, dental caries, abscesses, and tooth loss became more pronounced as high-carbohydrate, maize-based diets became the norm.11
The Cook
Mesoamerican skeletons also reveal that a settled way of life was hard on the joints and teeth. One way in which the Old and New Worlds differed was the latter's lack of beasts of burden (except the llama, which carried light loads) and technology which aided in strenuous tasks, such as the wheel or iron tools. Mesoamerica was a society powered largely by human muscle. Human bodies were the principle mechanism for growing food, erecting buildings, and transporting heavy burdens and goods. Hard and repetitive work imposed a severe toll on the bodies of both men and women, especially on the joints required for mobility, manipulation of objects, or bearing loads.9 Skeletal evidence from the Classic and Postclassic periods tends to show a higher occurrence of degenerative joint disease than populations from earlier times, reflecting the biomechanical stress that common people might have experienced when they shifted from a hamlet-like subsistence economy to an urban one based on trade. The wear and tear on Mesoamerican joints also reflects the division of work along gender lines. Women display significantly more joint disease of the wrists than men, not surprising given that the preparation of maize tortillas, the main source of calories, was a laborious task that had to be preformed twice a day by the women of the family. Men, the carriers of heavy loads, tend to show greater mechanical stress in the neck and lumbar region.10 Life based on agriculture also took its toll on the teeth of Mesoamericans. Although the dental wear and tear caused by the consumption of foraged foods was reduced over time, dental caries, abscesses, and tooth loss became more pronounced as high-carbohydrate, maize-based diets became the norm.11
7What kinds of infectious diseases might have afflicted the inhabitants of Mesoamerica? Skeletal evidence for tuberculosis and treponemal infection—forms of syphilis and yaws—have been found throughout the Americas, including Mexico.12 Whether or not this included venereal syphilis is still one of the most widely debated subjects in medical historiography, and one that I explore later in this chapter. It is likely, however, that some forms of venereal disease existed in Mesoamerica; "putrefaction of the member" is mentioned as a divine punishment for violation of ritual abstinence and medicines to treat male and female genitalia were listed in a native herbal.13 The most common aliments, however, were probably gastrointestinal and respiratory infections. These would have included things such as bacillary and amoebic dysentery, viral influenza and pneumonia, bacterial pathogens like staphylococcus and streptococcus, salmonella and other food poisoning agents, and various internal parasites. Shelburn Cook found that the Mexican materia medica indeed included an abundance of remedies for these types of illnesses. Based on the assumption that "any civilization relying upon an herbalistic rational of medicine inevitably tends to find a preponderance of medicines for those ailments that are both most common and most lethal," he compared Mexican remedies with those of contemporary Europe. His conclusion was that inflammatory and febrile infections were more prevalent in semi-tropical Mexico than in temperate Europe.14 Unfortunately, as soon as Europeans landed on the coast of Mexico in 1519, the extent and variety of Mesoamerican diseases increased rapidly, and with devastating consequences.
^topColonial Mexico
8Historians concerned with the story of disease in New Spain have centered their gaze, for the most part, on the horrific epidemics that nearly wiped out the indigenous population in the sixteenth century. Thanks to their work over the last thirty years, we have become more aware of the crucial role infectious diseases played in the conquest and colonization of the New World by Europeans. According to one of the pioneers of this field: "The fatal diseases of the Old World killed more effectively in the New, and the comparatively benign diseases of the Old World turned killer in the New."15 Scholars have shown comparatively little interest, however, in the endemic and chronic diseases of the day, which surely formed a greater part of everyday experience than the periodic outbreak of pestilence during which "normality" was suspended. One of the central assertions of this study is that the illness experiences of people in the past were very different than our own. Modern medicine has not only made enormous strides against infectious diseases—yesterday's great killers—but has significantly increased life expectancy, reduced our discomfort level from chronic disease and injuries through painkillers and highly technical surgical procedures, and medicalized death to such an extent that the passing of family and friends usually takes place away from our view and immediate experience. In contrast, the ubiquity of illness and, perhaps even more significantly, the likelihood of early death were simply part of the everyday landscape of the past, producing, certainly, a considerable effect on the mentalité of the time.16 Indeed, colonial sources for Mexico show that people were regularly watchful to all sorts of changes in their health and intensely concerned about the consequence of apparently trivial symptoms.
9We begin here our look at the broad spectrum of ill health that colonial Mexicans endured. So that we impose some kind of order over what is an otherwise haphazard collection of illnesses, we will start with the most clearly lethal diseases and work our way down to the less life-threatening ones. Our first foray into this world of sickness, then, will be the devastating epidemics that took so many lives, especially those of the native population in the first century of Spanish rule; next, we move on to the more common endemic illnesses that constituted an ever-present threat to the health of all novohispanos, or inhabitants of New Spain; and, finally, we end with a look at the everyday disorders that did not usually kill but proved to be, at best, troublesome nuisances and, at worse, extreme discomforts in this preanalgesic age.
^top"La mayor lástima del mundo"—Epidemic Illness
10The terror and defenselessness that people of past centuries must have felt toward epidemic disease is difficult for most of us to imagine. At the beginning of the twenty-first century, those of us that live in the developed world probably think our chances of dying from an infectious disease are fairly remote. The battle against contagious diseases, which began to make real progress after the First World War, has had great success in identifying innumerable deadly microbes and controlling them through vaccination and the use of antibiotics. Because the majority of us no longer die from infectious diseases, we now live long enough to develop chronic illnesses such as cancer, heart-related ailments, and Alzheimer's disease, making these the most feared maladies of our time. Such trends are clearly seen in twentieth-century Mexico. In 1930, 47 percent of deaths resulted from infectious diseases, while only 10 percent of deaths were attributed to these causes in 1990; likewise, deaths due to problems in the circulatory system (primarily heart disease) rose from 1.9 percent to 19.8 percent in the same years.17 The causes of these latest illnesses of civilization are closely linked to modern lifestyle—a surplus of cheap calories and increasingly inconvenient ways to burn them off—and the radically altered environment we live in; pathogens, although they may play a role in some cancers, are not viewed as significant factors in these diseases. In contrast, pathogens are still the most significant cause of morbidity and mortality in the developing world today. It is interesting to note that the one epidemic disease that has recently entered both the developed and developing worlds, AIDS, is viewed in the former as a disease of lifestyle—of homosexuals and drug users—even though most of its millions of victims in Africa and other parts of the developing world are neither. To view it as such is comforting because it implies that the individual has choices and thus control. Yet this sense of security, according to one researcher, may be a false one; the probability that new deadly diseases are awaiting the opportunity to invade the human species is great, with "AIDS appearing as merely the top of a viral iceberg."18 The illusion of control also tends to obscure the importance that lethal microbes have played throughout human history, an experience well illustrated by the European conquest of the New World, where "far more Native Americans died in bed from Eurasian germs than on the battlefield from European guns and swords."19
11The impact of Old World disease in the conquest of the New World is by now well known.20 The initial contact with Europeans was catastrophic for native peoples of America, causing perhaps close to 90 percent loss of life in some areas within the first century after contact.21 For the Valley of Mexico—the waterbound metropolis of Tenochtitlan-Tlateloco and other large settlements surrounding the lakes—estimates of depopulation in the sixteenth century range considerably. The largest estimate of population loss is as high as 97 percent, while the most conservative is about 60 percent.22 Accurate figures probably fall somewhere in between these two extremes, but whatever the numbers, the scale of population loss, especially in the first half of the sixteenth century, was truly staggering. Epidemic disease was clearly the dominant factor in the rapid population decline, although the harsh treatment and ecological devastation that accompanied Spanish colonialization certainly magnified the losses.
12New Spain suffered at least fifteen serious epidemics during the sixteenth century.23 Three of these are mentioned frequently in contemporary Spanish and Nahuatl sources, indicating them to be the most serious and widespread of the century's pestilential outbreaks: the well-known smallpox epidemic of 1520–1, and the great epidemics of 1545–8 and 1576–80, either one, or both, of which could have been typhus. By all accounts, the most devastating was the smallpox epidemic of 1520–1, during the siege of Tenochtitlan, allegedly introduced by a black slave fighting with the Narváez contingent. The illness spread quickly within the city and outward to areas still unvisited by the Spaniards, killing hundreds of thousands. The enormous military significance played by the pestilence was evident to both native and European chroniclers of the conquest. Smallpox demolished the native elite, destroying their diplomatic and military capabilities just as Cortés was preparing his final onslaught on Tenochtitlan.24
13The horror of this first pestilence comes through in several Nahua chronicles, the best-known of these being the account recorded by Sahagún in the General History of the Things of New Spain, his great encyclopedic enterprise on preconquest Nahua life. Book Twelve, a narration of the conquest, contains a vivid and melancholic description of the sufferers of smallpox:
. . . at the time the Spaniards left Mexico, there came a great illness of pustules of which many local people died; it was called "the great rash" [totomanaliztli or huey zahuatl].
. . . [The disease] brought great desolation: a great many died of it. They could no longer walk about, but lay in their dwellings and sleeping places, no longer able to move or stir. They were unable to change position, to stretch out on their sides or face down, or raise their heads. And when they made a motion, they called out loudly. The pustules that covered people caused great desolation; very many people died of them, and many just starved to death; starvation reigned, and no one took care of others any longer.
On some people, the pustules appeared only far apart, and they did not suffer greatly, nor did many of them die of it. But many people's faces were spoiled by it, their faces were made rough. Some lost an eye or were blinded.25
14
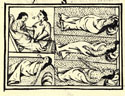 Nahuas infected with smallpox.
The text is accompanied by drawings of people suffering with the disease. Reclining and wrapped in blankets, they are covered with pustules, their agony registered in their faces and body positions. One patient is crying out in pain, while another is receiving consolation from a woman. Unlike the Spanish accounts of indigenous experience with pestilence, which tend to be more impersonal and interpretive, this Nahua account—less filtered, more visceral—comes closer to capturing the horror of their experience. Besides the physical suffering and overwhelming death toll caused by the severity with which the illness struck, the psychological shock must have been overwhelming because nothing like that had ever happened to native Mexicans.
Nahuas infected with smallpox.
The text is accompanied by drawings of people suffering with the disease. Reclining and wrapped in blankets, they are covered with pustules, their agony registered in their faces and body positions. One patient is crying out in pain, while another is receiving consolation from a woman. Unlike the Spanish accounts of indigenous experience with pestilence, which tend to be more impersonal and interpretive, this Nahua account—less filtered, more visceral—comes closer to capturing the horror of their experience. Besides the physical suffering and overwhelming death toll caused by the severity with which the illness struck, the psychological shock must have been overwhelming because nothing like that had ever happened to native Mexicans.
15
 Photograph of smallpox victim, with and without disease, 1896.
Smallpox is a horrific disease. It is extremely contagious; passed primarily through the air, a person can become infected just by inhaling a microscopic drop of the virus. Direct contact with any contaminated material, such as clothing or scabs, can also transmit the disease. After an incubation period of about twelve days, the victim develops a high fever, backache, vomiting, and severe malaise, followed shortly by the appearance of tiny red spots all over the body. These quickly turn into blisters, called pustules, which enlarge and eventually erupt as they become filled with pus. This eruption doesn't break the skin, but splits it horizontally, tearing away from its underlayers. The pain of the splitting is excruciating. At this point the patient either dies or the pustules dry up and form scabs which soon fall off, leaving disfiguring pox marks. It is believed that death is caused by a breathing arrest, a heart attack, shock, or a complete shut-down of the immune-system, but epidemiologist are still unsure how smallpox kills. The whole process takes about a month, after which a person is either dead or immune.26 The two photographs of a British smallpox victim in 1896—one showing the man infected, the other showing him in health—gives those of us who have never seen or experienced this disease a more vivid impression of its brutal effects.
Photograph of smallpox victim, with and without disease, 1896.
Smallpox is a horrific disease. It is extremely contagious; passed primarily through the air, a person can become infected just by inhaling a microscopic drop of the virus. Direct contact with any contaminated material, such as clothing or scabs, can also transmit the disease. After an incubation period of about twelve days, the victim develops a high fever, backache, vomiting, and severe malaise, followed shortly by the appearance of tiny red spots all over the body. These quickly turn into blisters, called pustules, which enlarge and eventually erupt as they become filled with pus. This eruption doesn't break the skin, but splits it horizontally, tearing away from its underlayers. The pain of the splitting is excruciating. At this point the patient either dies or the pustules dry up and form scabs which soon fall off, leaving disfiguring pox marks. It is believed that death is caused by a breathing arrest, a heart attack, shock, or a complete shut-down of the immune-system, but epidemiologist are still unsure how smallpox kills. The whole process takes about a month, after which a person is either dead or immune.26 The two photographs of a British smallpox victim in 1896—one showing the man infected, the other showing him in health—gives those of us who have never seen or experienced this disease a more vivid impression of its brutal effects.
16Mortality rates of this first epidemic can only be guessed at since contemporary estimates are crude and impressionistic. According to the friar Motolinía, one of the first Franciscans on the scene, "in some provinces half the people died, and in others a little less"; another Spaniard, a participant in the siege of Tenochtitlan, put the death rate at "more than one-fourth."27 Because this was a "virgin-soil" epidemic, rates of infection could have been as high as 100 percent, with death rates of one-third or higher.28 The severity of the smallpox epidemic of 1520–1 is easily explained by the New World's long isolation from the rest of mankind and evolutionary differences between the two areas in the development of pathogens. Pre-Columbian populations had no previous exposure to the crowd diseases that had forced the immunological systems of Old World peoples to erect defenses because they had completed their migration to the Americas by 10,000 BC, well before epidemic diseases had been established in the Old World. Throughout the course of conquest, the immunologically naïve inhabitants of the New World came in close contact with the "immunological supermen" of the Old World. Among the Europeans, it might be argued that the Iberians possessed one of the most evolved immunological systems in the world at that time. The peninsula had long been a crossroads of European and Arabic civilizations, and its roads had carried myriad peoples and their diseases for centuries. The cities of Iberia, where sewage and garbage flowed through the streets, abounded in disease-carrying rodents and insects; Iberians bathed infrequently, and their skin, hair, body fluids, and breath swarmed with pathogens. Exposed routinely to a host of childhood ailments, such as smallpox, measles, and mumps, their immunological systems indeed made them seem superhuman in the eyes of the natives being destroyed incomprehensibly by pestilence.29
17The rise of epidemic disease in human history parallels the rise of civilizations. As long as humans lived in small isolated groups—nomadic hunter-gatherers, for example—their ailments were limited to chronic illnesses of low infectivity. Diseases that we tend to associate with large-scale epidemics, such as measles, smallpox, mumps, and pertussis can not sustain themselves in small populations. Lacking the essential antibodies, these groups could be wiped out entirely by an infected outsider, which in turn would kill the pathogens themselves, as they can only survive in the bodies of living people. Small population size helps explain not only why such groups could not sustain acute infectious diseases, but also why they could not evolve epidemic diseases of their own to give back to outsiders. In addition, small bands of hunter-gathers rarely remained in an area long enough to foul their water supplies and build up the refuse that would attract varmints that carry diseases and the vectors that spread them. Nor did these groups have the domesticated animals from which so many of the later crowd diseases originated. This is not to say that small human populations did not develop infectious disease. They did, but only of a certain type: those diseases in which the host can remain infected for a long time, such as amoebic dysentery, leprosy, and yaws, or those diseases that have microbes that can maintain themselves in alternative hosts, like water or insects, such as schistosomiasis or yellow fever. These groups were also susceptible to non-fatal infections to which humans do not develop lasting immunity like the common cold, flu, and internal parasites.30
18Sedentary agriculture and the subsequent growth of cities expanded human populations to a density that could support very acute and very transient infections. Rapid transmission and acuteness are what give crowd diseases their terrible lethality. In a simplified form, epidemics work like this: microbes spread very rapidly within a local population, infecting almost everyone; victims either quickly die or recover and become immune, leaving no more infected people. Because the microbes cannot survive except in human bodies, the disease dies out for the time being. With the birth of new and non-immune, generations, the local population again becomes susceptible to diseases carried by an infectious visitor from outside, thus starting a whole new epidemic cycle.31
19The one-sidedness of the exchange of lethal pathogens between the Old and New Worlds is striking. Although over a dozen major infectious diseases were imported into the Americas by Europeans, perhaps not a single significant disease was passed to Europe from the New World. The one possible exception is syphilis, although its origins are still being debated. Yet, how is it possible that densely populated areas of the New World like Mesoamerica, the Andes, and the Mississippi Valley did not develop crowd diseases of their own? The most likely answer is that they had very few domesticated animals from which these diseases could evolve. Old World crowd diseases evolved out of the illnesses of herd animals that became domesticated; cattle, sheep, goats, dogs, pigs, horses, and fowl all contributed their pathogens to swelling pools of disease. People lived closely with these creatures, sharing water, air, and sometimes shelter with them. Thus, pox viruses were passed back and forth between humans and cattle to produce smallpox and cowpox, whereas the exchange and combination of different strains of viruses among dogs, cattle, and humans created distemper, rinderpest, and measles. The scarcity of domesticated animals in the Americas reflects the small number of wild animal candidates for domestication. Nearly 80 percent of its large wild mammals became extinct after the last Ice Age, about 13,000 years ago. Only five animals are known to have been domesticated in precontact America: the turkey in Mesoamerica, the guinea pig and llama/alpaca in the Andes, the Muscovy duck in tropical South America, and the dog throughout both continents. Yet none of these animals appear to have been likely sources of crowd diseases. Humans do not have much physical contact with Muscovy ducks and turkeys, nor do these fowl live in huge flocks. Guinea pigs, which do live closely among people, may have been the source of Chagas's disease or leishmaniasis, extremely unpleasant maladies, but not crowd killers. Nor did llamas and alpacas, the only comparable form of indigenous livestock found in the Americas, contribute to human disease pools, unlike cattle and sheep.32 According to one researcher, the cameloids had four strikes against them as a source of human pathogens:
[Llamas] were kept in smaller herds than were sheep and goats and pigs; their total numbers were never remotely as large as those of Eurasian populations of domestic livestock, since llamas never spread beyond the Andes; people don't drink (and get infected by) llama milk; and llamas aren't kept indoors, in close association with people. In contrast, human mothers in the New Guinea highlands often nurse piglets, and pigs as well as cows are frequently kept inside the huts of peasant farmers.33
Thus, the animal origins of human disease lie behind some of the broadest patterns of human history. For Native Americans, this chance aggregation of factors was momentous, as events in sixteenth-century Mexico so starkly demonstrate.
20The smallpox epidemic of 1520–1 has become such a familiar component of the conquest narrative that subsequent epidemics tend to get slighted in the attention they get from historians. The two other major outbreaks of pestilence during the sixteenth century were probably as costly in terms of human life as the first one and had equally dire consequences for the indigenous communities that suffered them. Spanish writers who witnessed the epidemics of 1545–8 and 1576–80 were astounded by the tremendous number of dead.34 Sahagún writes:
In the year 1545 there was a huge and universal pestilence where, in all of New Spain, most of the people who lived there died. At the time of this pestilence I was in Mexico City, in the part of Tlateloco, and I buried more than 10,000 bodies, and at the end of the pestilence I became ill and almost died.35
 Epidemic of 1544–45
Indigenous sources chronicle these events as a great cocoliztle, (great plague or illness) in various codices. The Códice Telleriano-Remensis, for example, records the epidemic of 1545–8 with paintings of cadavers wrapped in straw mats and bundled together. Linked by lines to glifs representing those years, the accompanying gloss states: "[in the] year of 1544 and of 1545 there was a great mortality among the Indians."36
Epidemic of 1544–45
Indigenous sources chronicle these events as a great cocoliztle, (great plague or illness) in various codices. The Códice Telleriano-Remensis, for example, records the epidemic of 1545–8 with paintings of cadavers wrapped in straw mats and bundled together. Linked by lines to glifs representing those years, the accompanying gloss states: "[in the] year of 1544 and of 1545 there was a great mortality among the Indians."36
21The epidemic of 1576–80 is especially rich in documentation; for a variety of reasons, many reports were compiled around this time, so mention of it is common. Several of the Relaciones Geográficas offer commentary about the epidemic and its destructive effects on a population already reeling from more than fifty years of contact with European diseases. The Relación de Cuauhiquilpan, for example, states that ". . . in this pueblo there are very few Indians at the present time: there used to be more than five hundred Indians of tribute, but about four years ago many died of the pestilence, so that now it seems no more than fifty remain."37 A sudden drop in population had far-reaching consequences in the new colony; it meant that there were no longer people available to work the fields and orchards, and many communities fell into ruin. Antonio de Ciudad Real, traveling during the years 1584–9 through Mexico with Fray Alonso Ponce, a Franciscan commissary-general, notes how one community was reduced to ruin by the epidemic:
In times past that town had a large population, according to the older people and now it just seems like ruins of houses, and for the many fruit trees there are in the surroundings, among which the Indians usually have their towns, especially being in the hot lands, like it is, but with the cocolitzle, there was such a very large pestilence and mortality in that land, that everything was destroyed and now there are scarcely two hundred inhabitants.38
The impression that things had fallen into a state of disintegration was widespread throughout all of New Spain. Spaniards, for the most part, were spared from these early epidemics, but they must have been truly shaken as they watched their labor force die off like flies ("como chinches" said one source).39 One of the most poignant descriptions of this experience comes from a letter written during the epidemic by a hacienda owner to an acquaintance in Spain. His estate has fallen into a state of idleness for lack of workers, and he appears frightened and overwhelmed by the magnitude of death he sees around him. The pestilence, he says, is "la mayor lástima del mundo," the greatest sorrow of the world.
. . . at the present time there has been and still is a pestilence among the natives so widespread and so terrible that it is the greatest sorrow of the world, and in the province of Tlaxcala, where I live, they say that more than 80,000 people have died, and at our hacienda we have lost more than 200 people, and among those some blacks, and for this the work of the hacienda has stopped and we are all trying to do what we can, giving orders to find people, but none can be found. . . . God in his mercy has guarded the Spaniards, because until now only a few of them have died, but we are in great fear . . . and so everyone here is with great necessity, because the wealth of this land are these Indians, because, as there are so many, they provide service and work, and as so many of them have died, everything has stopped.40
22What diseases could have caused such staggering population loss? Various modern scholars, beginning with Alexander Von Humboldt at the turn of the nineteenth century, have sought the answer to this question, but no clear consensus has emerged. The identification of diseases from historical descriptions is a dubious task. Specialists usually have to work from contemporary records of symptoms, which can be a problem since descriptions are often vague and in many cases the same symptom could result from different illnesses. Even for the most clearly and widely described illnesses, such as smallpox or typhus, it is often difficult to make an exact diagnosis because the circumstances that favor the spread of one type of illness can create opportunities for the transmission of another, thus creating multiple epidemics in a community at the same time. This, in turn, frequently produces a confusing record of symptoms.41 Humboldt identified the pestilence in 1545–8 as matlazáhuatl, a Nahua term that came to be associated with typhus sometime after the middle of the sixteenth century.42 Other scholars appear more skeptical about assigning an identity to this epidemic. Contemporary sources, both Spanish and indigenous, failed to call the disease by any name, neither tabardillo—the Spanish name for typhus—nor matlazáhuatl.43 Mendieta, for example, wrote that both epidemics were due to "pujamiento de sangre," or "full bloodiness," but that the illness of 1576 was also tabardillo.44 One of the most striking symptoms recorded for both epidemics was bleeding from the nose. The Códice de 1576, for example, states: "In August came the pestilence, blood came from our noses, we made our confessions to the friars and they gave us permission to eat meat, the doctors cured us." One of the illustrations accompanying the Nahuatl text shows a person bleeding copiously from the nose.45
23Other symptoms are vividly described in the Relación de Ocopetlayuca, a small corregimiento located on the southern slope of Popocatépetl in the present-day state of Puebla, which lost over a third of its inhabitants in the 1576–80 epidemic. An eyewitness reports that:
. . . it is the nature of this illness that it causes great pain in the "mouth of the stomach" with horrible fever in all parts of the body and head, and those that die, do so within six or seven days; . . . the ones that survive become healthy, although sometimes the illness attacks them again and they die. No medicine is effective against this disease.46
That this was an outbreak of typhus is further suggested by later comparisons of it to another severe epidemic, that of the great matlazáhuatl epidemic of 1736.47 But an accurate diagnosis of the illnesses behind these epidemics may never be known. Sources fail to mention the rash that is characteristic of typhus, and the most conspicuous symptom reported, bleeding from the nose, does not figure among presently known symptoms of the disease. Yet the magnitude of death in both epidemics has made typhus a plausible explanation because its potential lethality is as great as smallpox, measles, or plague, any of which would have been easily recognized at this time.
24Like smallpox, typhus can be an extremely acute illness in its epidemic form. In a typical course, onset can begin abruptly with a very high fever, severe headache, extreme weakness, and general malaise. A rash appears on the fourth or fifth day, usually starting on the shoulders and trunk, and sometimes spreading to the extremities, although it rarely appears on the face. This is not a blistery rash, like that of smallpox, but one of barely raised spots, ranging from two to five millimeters in diameter. Both its Nahuatl and Spanish names refer to its distinguishing rash: matlazáhuatl, a composite of matatl, meaning "net," and záhuatl, indicating "eruptions" or "rash," thus a "net-like rash"; and tabardillo (or sometimes tabardete) in reference to the rash covering the body like a "tabard," or sleeveless cloak. In fatal episodes, the patient becomes completely debilitated, falls into a coma, and dies of cardiac arrest; mortality rates can be as high as 25 percent. In contrast to the smallpox virus, which cannot survive outside living human bodies, typhus is transmitted to people by insects. Several of the Old World epidemic diseases transferred to the Americas were spread by anthropoids such as lice, fleas, and mosquitoes. Malaria and yellow fever—both well-known illnesses spread by mosquitoes—have been endemic, and sometimes epidemic, in many parts of tropical America since the sixteenth century. The port of Vera Cruz, for example, was a dreaded stop for travelers because of its seasonal outbreaks of yellow fever. Like the bubonic form of plague, the typhus virus is carried by rats in their fleas, which explains how the disease persists between outbreaks. Humans can contract the endemic form of typhus from the bites of rat fleas. An epidemic results when people begin to transmit the virus among themselves, which happens if they are infested with body lice. The body and the head louse, which travel easily among people in crowded conditions, take up the virus from the infected blood of one victim, and leave it on the skin of another by way of their feces. The virus enters the body through abrasions in the skin, such as scratched insect bites, and the process of infection begins its cycle. Typhus confers an immunity on its survivors, which, though not permanent, may last for years. Early modern Spaniards only became familiar with the epidemic form of typhus at the end of the fifteenth century, when it first appeared during the battle for Granada in 1489–90. Hans Zinsser, who wrote a history of typhus during the 1930s, believed that the disease was brought to Spain by soldiers from Cyprus, where it was prevalent. It struck the Iberian Peninsula repeatedly during the sixteenth century, and it gradually spread to the rest of Europe, assisted chiefly by the march of armies. Just how and when typhus entered the New World is still not known, but in all likelihood it was transported by infected rats aboard ships from Spain.48
25Epidemic diseases periodically assaulted the inhabitants of Mexico throughout the colonial period and well into the nineteenth century, although the extent of population loss during subsequent epidemics was never as great as in the sixteenth-century episodes. The one exception may be the great epidemic of matlazáhuatl of 1736–9, where it was estimated by an eyewitness that more than a third of the inhabitants of Mexico died.49 In addition to smallpox and typhus, measles, mumps, scarlet fever, whopping cough, and yellow fever all remained endemic in parts of New Spain between their periodic appearances as pestilence. These highly contagious diseases, very often referred to simply as "la peste," were the most feared by all sections of the population, regardless of their social class or race. The ex-voto of Doña Luisana, with which I opened this chapter, not only gives us a pictographic starting point for imaging the experience of a smallpox victim, but also poignantly affirms the old adage that every statistic conceals real personal misfortune. During the years 1761–2, most of New Spain had been in the grip of smallpox and typhus, which had swept through the colony killing thousands. No firm mortality rates are known but one contemporary estimate put the death toll in Mexico City alone at around 25,000 people.50 The date of Doña Luisana's ex-voto, the winter of 1761, confirms she was part of this epidemic, and her location, Cholula, a city just outside of Puebla, would have placed her in a densely populated area of Mexico, where infectious diseases could freely run their course. The painted scene portrays the sufferer as an upper class woman; although the room is simple, the sick-bed appears to be outfitted with costly, decorative linens and the people attending the patient are dressed quite formally, especially the men. Doña Luisana "being sick from smallpox, and very dangerously so," languishes in her sick-bed, her skin completely covered with a frightful rash, although she appears to be well attended by caregivers. That this sufferer survived her ordeal is evident from the ex-voto itself, as it was produced to show gratitude for "the marvels" the divine images in it bestowed on the patient.51 This ex-voto is vivid testimony that la peste was a category of illness to be feared above all else, a sentiment also poignantly expressed in letters the Condesa de Miravalle wrote to her son-in-law, Pedro Romero de Terreros, around this time. She implores her family to be mindful of their diet and extra vigilant about guarding the children's health, . . . "the epidemic raging here, which spreads wherever it enters and leaves no one alive, is worse than the smallpox."52
26There is little doubt that epidemic disease (with the possible exception of infant mortality) was responsible for most premature deaths throughout the history of New Spain. Frequently these were "compound epidemics" in which the appearance of one disease triggered others latent in the population, creating a combination of disease agents with often disastrous results. These pestilential invasions, for which there were no known effective treatments, were so varied in character, and so widely dispersed in time and space that all inhabitants, white or native, rich or poor, young or old, were threatened by them at some time in their lives. The bulk of epidemic victims, however, were disproportionately from the lower groups in the socioeconomic order—in New Spain, this meant the vast majority of the population, almost all of them Indians and mestizos. This ancient affinity between poverty and disease was intensified by the fact that epidemics frequently ran in cycles that paralleled widespread crop failures, generating the twin scourges of sickness and famine.53 Over the years, various lists have been compiled of these pestilential crises. Writing in the eighteenth century, Cayetano Cabrera y Quintero chronicles eighteen major epidemics from 1520 to 1737, and notes the extremely high mortality rate among Indians, for which he attributes their poverty, excessive drinking of pulque, and an intense fatalism in the face of death. Gibson's list of colonial epidemics is extensive: apart from fifteen in the sixteenth century, he catalogs thirty-five more for the remainder of the colonial period.54
27In the last century of colonial rule, smallpox erupted into epidemic form every fifteen to twenty years, with enormous loss of life. In 1798, the Spanish king, Charles IV, ordered a massive vaccination campaign for all of Spain's colonies, and, in 1804, Jenner's vaccine became available in Mexico for the first time. Popular acceptance of the new procedure was widespread and mortality was greatly reduced, but in the turbulent nineteenth century, vaccination campaigns were practiced intermittently, thus ensuring that smallpox would not be eradicated from Mexican soil for another century and a half.55 Unfortunately, at the turn of the nineteenth century, the same optimistic prospects did not hold true for that other killer of the colonial period, the louse-borne disease of typhus. This is not surprising given the inadequacies of public and private hygiene practices of the time and the state of medical knowledge, which still did not fully understand the causal relationship between filth and disease.
^top"Quebrantada de salud":—Endemic Illness
28Although epidemics show up as distinct peaks of mortality in the historical record, making them fairly visible to the researcher, the range and scale of endemic disease is more difficult to discern. Yet colonial sources are full of testimonies about the more frequent illnesses afflicting people, especially those that manifested themselves with gastrointestinal symptoms. One chronicler noted that as Fray Alonso Ponce was making his way, on foot and horseback, through New Spain during the 1580s, he was overcome by "vomiting, so severe and of such quantity of black humor, that the official [he was traveling with] became terrified." When asked to record which diseases were most prevalent in the towns of New Spain, the authors of the Relaciones Geográficas cited cámeras de sangre ("bloody diarrhea") more than any other illness. And, in a letter she wrote in July 1757, the Condesa de Miravalle remarked to her son-in-law that she was "bien quebantada," that is, her health was "broken" as she had just endured an episode of "dark vomit" and now was suffering from a severe cough.56 Colonial Mexicans mention los vómitos and las cámeras so often in their writings, there can be little doubt that gastrointestinal ailments were the most ubiquitous of maladies. Equally universal, too, were the illnesses that involved the respiratory system; then, as now, everyone suffered their fair share of head colds, coughs, mal de pecho, and sore throats, along with more serious respiratory ailments. Although these two sets of symptoms, gastrointestinal and respiratory, could stem from any number of diseases, many of them deadly, they often were viewed as illnesses in and of themselves.
29Juan de Cárdenas, writing in the sixteenth century on various aspects of the people and animals born in the Indies, comments on the ubiquity of stomach problems in New Spain. "Certainly . . . in the Indies, there is scarcely a man that does not go around complaining of his stomach, no matter whether he be old or young, man or woman, born in the Indies, or recently arrived from Spain . . ."57 This same observation is made by Fray Agustín Farfán, a doctor who wrote a popular book on domestic medicine late in the sixteenth century. His first chapter is devoted to flaqueza de estomago ("weakness of the stomach"). Like Cárdenas, Farfán notes the many people who seem to suffer from this malady: "It is very sad to see in New Spain the many that complain of weak stomach, and of not being able to digest their food, even when they have eaten little."58 Both authors were writing about the Spanish population of New Spain which seems to have suffered from an array of gastrointestinal problems. Farfán is very specific in his descriptions of the symptoms:
Some eat what appeals to them and what their stomachs desires, even though they can not digest it. Others vomit what they eat along with a great quantity of putrid and acidic humors. Others throw up and belch gas all day long, and spit up phlegm and they vomit curds that are clear like egg whites.59
30Just why Europeans would have endured a myriad of digestive problems is given a great deal of attention in both these works, and rightly so as the stomach played a pivotal role in the humoral view of how the body worked, something that will be explored in chapter four of this book. New immigrants would have undoubtedly encountered a host of gastroenteric pathogens to which they would have had no immunity, causing them stomach problems and diarrhea just as modern travelers do today. Many Spanish emigrants in their letters to family and friends back in Spain complain of being sick. Alonso de Alocer, writing to his brother in Madrid complains: ". . . since coming here I have not had one day of health, because everyone that comes here from Spain gets chapetonada and more than a third of those that come die of it." The chapetón (recently arrived Spaniard), was vulnerable to sudden illness and death, as many of these letters confirm. One letter writer informs an acquaintance in Jaén that his brother in Mexico City has died suddenly from diarrhea, whereas another informs her daughter in Sevilla that "God has been served" by taking the life of her husband, who died from "diarrhea, along with fever."60
31Diseases of the respiratory tract also were prevalent. Contemporaries called these illnesses by a variety of names: romadizo, catarro, tos, tos antiqua, pasmo, hinchazones en la garganta, and asma. More serious respiratory infections were also common. One that is mentioned in many of the domestic medicine manuals and in contemporary descriptions of illness is dolor de costado, literally, "pain in the side." Both Farfán and Esteyneffer describe this disease by listing its most common symptoms: the patient feels a very sharp pain in one of his sides, has a high fever, has great difficulty breathing, a persistent cough, and "hard" pulse. "When all these symptoms and signals are present," writes Farfán, "then dolor de costado is very dangerous, and can kill quickly, depending on the state of the patient." He later states that the first thing an attending physician should do is to make sure the patient has made confession and has "put his soul in order."61 Juan de Brihuega, an inhabitant of Puebla in the sixteenth century, almost lost his pregnant wife to this disease; she was so sick that "they bled her six times, and because of this, she almost died."62 Dolor de costado must have specified a large group of symptoms common to many actual diseases, such as pleurisy, emphysema, pneumonia, or tuberculosis.
32People often simply described their illnesses by it most prominent symptom, calentura, or fever. In the town of Cuicatlán, the Indians tend mostly to be sick from "fevers, because it is very hot there . . ." and in the nearby pueblo of Tututepetongo, "they sometimes get some fevers, which they cure with wild maguey leaves."63 Both the Nahua and European medical systems recognized different types and qualities of fevers; contemporaries called them by various names: tercianas, cuartanas, calentura hética, calentura continua. Marco Ortiz wrote to his father in 1569 that he had been very ill "with chills and double tertian fever (tercianas dobles) that lasted for six months, [after which] I was cured, God being served." Antonio de Ciudad Real happily notes the day, in Tratado curioso, when he realized that he was finally free from quartan fever (cuartanas), which had plagued him for more than three years.64 Intermittent fevers like these were probably malarial, and these two cases could very well have originated in Spain, as their carriers had only recently arrived from the Peninsula. Each of the different species of malarial parasites have their own periodicity. For example, the parasite causing benign tertian malaria, Plasmodium viva, has an incubation time of about ten to seventeen days; the resulting fever, which can be as high as 104–106 degrees Fahrenheit, lasts for two to six hours and recurs every third day. In contrast, the incubation period for quartan malaria, caused by Plasmodium malariae, can be as long as thirty or forty days, with fever coming every fourth day. These episodes of fever are usually accompanied by nausea, vomiting, diarrhea, and, at the end of the attack, profuse sweating. Both types of malaria, if left untreated, can last for months; as the disease progresses, the spleen enlarges, and the patient becomes anemic and sometimes jaundiced.65 That malaria was present in New Spain is well known—it proved quite destructive to coastal Indians in the early colonial period—but whether it preceded the Spaniards is still a matter of dispute. Those well-versed in precontact medicine say that the Nahuas were familiar with intermittent fevers and came to distinguish them by their pattern of onset and recurrence.66
33Another mosquito-borne illness that claimed many victims in the colonial and early national period was yellow fever. Endemic in the coastal areas of Mexico until its eradication in the early 1920s, this disease, which could well have been the "Montezuma's Revenge" of its day for the way it seemed to attack only Europeans, is forever linked to the history of Veracruz. As the region's only serviceable port, the coastal city was established soon after the conquest, not as a desirable location of Spanish settlement, but as a necessary link between New Spain and the outside world. Shortly thereafter, inbound Spanish passengers, who had no choice but to pass through the insalubrious city, were calling this place la tumba de los españoles, for its horrible association with pestilential fevers. By the eighteenth century, travelers and residents alike attributed the many deaths to one disease in particular: el vómito prieto, or as it came to be known in the late colonial period, fiebre amarilla.67 One traveler, the indefatigable Capuchine friar, Francisco de Ajofrín, had this to say about the horrors of the illness:
The terrible disease that has been suffered by this city (although now somewhat alleviated) is the "black vomit," which is vomit of black blood and putrefaction. This formidable contagious disease, which has buried in an infinite number of Europeans, does not bother the Indians with any regularity, and so it really belongs to those who come from the other side. . . . The first signs of this illness is the vomit itself and symptoms so mortal and expeditious, that many die on the first day; others, on the second or third; it being rare that any escape; nor have the study and effort of many doctors and surgeons, of the fleets or shore, [who have] examined this disease with great diligence, been able to find any medicine to prevent or cure it.68
34Although the symptoms of yellow fever can be quite mild—some victims recover unaware of ever having contracted the disease—the more serious forms can be horrific and life-threatening. Nausea, high fever, and severe headache set in usually three to six days after the initial infection. As the disease advances, the liver becomes damaged, causing the two most distinctive indications of yellow fever: jaundice and bleeding from the gums, nasal passages, and stomach lining, which is exacerbated by the liver's inability to make essential factors needed by the body's blood-clotting system. The severe gastrointestinal bleeding causes frequent, and at times violent, hematemesis (vomiting of blood), and it was this symptom that earned the sickness the name of vómito prieto. Among these more serious cases, mortality can be as high as 50 percent. Death comes quickly after the appearance of renal failure, convulsions, and cardiovascular collapse, usually seven to ten days after the initial onset of symptoms.69
35If the phenomenon of Indians succumbing to smallpox while Spaniards were unaccountably spared was baffling to contemporaries, equally mystifying was the way in which yellow fever struck Europeans while the native population remained largely unaffected. In the nineteenth century, Southerners in the United States referred to this same illness as the "stranger's disease" because it appeared to attack only visitors from the northern states or Europe while inexplicably sparing long-term residents, both blacks and whites. In Veracruz, lifelong residents had little to fear from yellow fever, which seemed solely to afflict recent arrivals on the incoming ships or highlanders descending to the coastal region. This occurred because the city provided a perfect conflux of disease-prone conditions. The heavy rainfall and year-round warm temperatures offered an ideal environment for a thriving mosquito population; the two types known to carry the yellow fever virus in Latin America, Haemagogus and Aedes aegypti, flourished here.70 According to one historian, Veracruz itself provided a perfect setting for the latter, which breeds preferentially in small bodies and containers of water.
Drainage in the rain-soaked town was notoriously poor. Heavy showers left alleyways and plazas inundated with water for days, even weeks. Street puddles combined with household pots and vases and the large cisterns that stored drinking water in wealthier homes to give the periodomestic mosquito ample opportunity to spawn during the wet summer months.71
36Longtime residents of areas where yellow fever is endemic are unlikely to experience dramatic outbreaks of the disease because exposure early in life, usually resulting in milder cases of infection, confers immunity from later infection. Yet, as New Spain's only Atlantic port, Veracruz's streets were frequently filled with a large susceptible host population. Each year, the Spanish flota brought hundreds of immigrants with no prior exposure to the yellow fever virus, along with scores of equally vulnerable highland residents who descended to meet them and the goods brought by the ships. And, after 1778, when Charles III liberalized colonial trade laws, the economic opportunities in Veracruz attracted newcomers from both sides of the Atlantic. Thousands of comerciantes, peddlers, artisans, day laborers, muleteers, and sailors from Spain and the interior of Mexico entered the mosquito-infested harbor with little or no immunity from the virus. That vómito prieto would infect hundreds, if not thousands, of people almost every year was virtually assured by one more factor in this convergence of conditions: seasonal weather patterns in the gulf coast. Because of their breeding and lifespan cycles, the mosquito population reached its peak in August and September, well after the onset of summer rains. Coinciding with this infestation were the arrivals of the ships from Spain. The flota bound for Mexico left Seville in early to mid-summer, crossed the Atlantic via the Canaries, and entered the port of Veracruz in late summer or early fall, usually just in time to avoid hurricane season and the arrival of the northern winds, los nortes, that made navigation in the gulf so treacherous.72
37The cycle of sickness that descended on Veracruz every year ended rather abruptly in late fall as the northern winds literally swept the threat of disease from the port. Because aedes aegypti is a weak flier, strong winds can push the mosquitoes far from their preferred habitat.73 The arrival of the nortes coincided with the end of the rainy season, curtailing the breeding of any remaining mosquitoes until a new cycle could begin the following spring.
38Although the more visible infectious diseases produced high levels of morbidity and mortality in the colonial population, other illnesses, of great consequences but less visible as causes of death, also took their toll. Modern paleopathological analysis of skeletons disinterred from beneath the Metropolitan Cathedral of Mexico City have revealed some interesting data on the health of colonial inhabitants. In addition to the more predictable findings, such as the prevalence of osteoarthritis, osteomyelitis, and many bone fractures caused by trauma, the study revealed a surprisingly high incidence of two diseases: scurvy and syphilis.74
39Scurvy, a disease caused by a lack of vitamin C, was first recognized to be a major problem for Europeans in the late fifteenth century, a period that coincided with technological advances in shipbuilding that allowed for very long sea voyages. Because the human body cannot produce ascorbic acid endogenously, it is completely dependent on dietary sources—mainly fresh fruit and vegetables, and to a much lesser extent, fresh meat—for the vitamin. Salted or dried meats (these curing methods result in the loss of the vitamin), grains, nuts, eggs, and dairy products provide little or no vitamin C. Scurvy is a serious disease, one that can easily kill its victim if left untreated. The lack of ascorbic acid impairs the body's ability to manufacture collagen, an essential glycoprotein component of connective tissue. Scurvy first appears in vitamin-deficient individuals in about twelve weeks, causing extreme fatigue and lethargy. After some seventeen to twenty-six weeks without consumption of vitamin C, the more severe symptoms set in: hemorrhagic spots under the skin, softening of the gums, and defective wound healing. The traditional diet on long voyages—wheat flour, salted meat, oatmeal, dried peas, oil, and cheese—was almost totally lacking in vitamin C. By the end of the fifteenth century, long-distance travel by sea had become more common, meaning that people could now stay at sea for months at a time, long enough to suffer the deleterious effects of not having an adequate supply of fresh fruits and vegetables. One researcher has estimated that at least one million seamen died from this disease between the years 1600, when long voyages had become more common, and 1800, when the protective effects of lemon juice became known. "In this sense scurvy . . . may truly be regarded as one of the earliest occupational diseases."75
40The effects of scurvy, or escorbuto, on seamen are vividly described by Antonio de la Ascension, a priest who accompanied an expedition from Mexico in 1602 to explore the coastline of California. When the ship was delayed by adverse winds, the crew members began to develop some alarming symptoms, such as body aches, large purple spots covering the body, severe stiffening of the legs and thighs, extreme swelling of the gums "to such a size that neither the teeth nor the molars can be brought together . . . [and] the teeth become so loose and without support that they move while moving the head." With this disease, the victims "come to be so weakened . . . that their natural vigor fails them, and they die all of a sudden, while talking." The writer also noted that the mysterious disease broke out in the same place that the Spanish fleet, coming back from the Philippines to Mexico each year, experienced the same problem. He concluded that the winds of that area are "so sharp, subtle and cold" that they "pass through thin men." These winds, he continued, carry with them "much pestilence, and if in itself the air is not bad, it produces with its subtlety and coldness some corruption of bad humors, especially in persons worn out and fatigued with the hardships of the navigation." Some of the crew survived the trip to California because a forced landing was made in Mazatlan where some of the ship's members discovered a cactus fruit that grew in abundance there. The acidic fruit, along with the efforts of the Virgin del Monte Carmel, restored the health of those on board fairly quickly.76
41Although evidence of scurvy was most clearly seen among sailors on long voyages, it should be remembered that it also affected early modern urban populations; the inhabitants of European cities frequently suffered from this malady.77 That evidence of scurvy was found in skeletal remains from the Cathedral's cemetery is understandable when we recall that only people of Spanish origin are likely to have been buried there. Most criollos—the American-born descendants of Spanish immigrants—were urban residents and probably had diets that lacked a variety of fresh fruits and vegetables a good deal of the time. During the colonial years, too, escorbuto was often associated with dental conditions and with venereal disease. One remedy from the eighteenth century, advertised in the Gaceta de Mexico, promised to "clean, whiten, and fortify the teeth," and also to cure scurvy. Another praised the virtues of two types of agave plants that were useful in the treatment of venereal disease and scurvy, and "other diseases which do not respond to the use of mercury and other known remedies."78
42There is much evidence that syphilis was also a major health problem among New Spain's population, especially in the sixteenth century when, because of its newness, the disease struck with a virulence it was to lose in later centuries. If sufferers of bubas, as the disease was then commonly called, were thick on the ground in the new colony, so were a myriad of healers peddling remedies for this affliction. In 1527, one of the first acts of the new Ayuntamiento was to issue an order prohibiting unlicensed practitioners from treating "those that are sick with bubas and other sores or pains. . . on penalty of sixty gold pesos for each time done to the contrary."79 In the 1540s, the bishop Juan de Zumárraga erected the Hospital del Amor de Dios primarily to care for syphilitics; the medical staff of eighteen included four untadores—people who applied the mercurial unguents that were the standard treatment of the day.80 Medical writers in the sixteenth century seemed particularly interested in this disease—its origins, its bewildering variety of symptoms, and its treatments, especially those coming out of the New World. Pedro Arias de Benavides devoted almost his entire Secretos de cirugía to the diagnosis and treatment of morbo gálico, the French disease, which was the other favored appellation of the time. In his treatise on medicine, Farfán expressed "great sorrow for those I see each day who die of the sickness of bubas"; he warns his readers there are many who claim to know how to cure this illness, but end up leaving their patients "worse than when they began the cure." He continues with advice on how to recognize and treat the disease with various substances and techniques such as sarsaparilla, guaiacum, various ointments, and fumigation. Juan de Cárdenas, in his typically florid language, also had much to say about the disease; his claim that syphilis was more widespread in New Spain than anywhere else in the world is certainly hyperbolic, but does give a sense of the magnitude of the problem.
Among the diseases, because of our recent faults and recent sins, that have lately found and tested the human body, one of them, the Indies disease, or, according to others, the French disease, is so infernally malignant and pernicious, that it truly afflicts, oppresses, and torments men, without any exception. It is now even commonly said in the Indies that one is not an honored man if he does not carry in his face a sign or trace of this sickness. Thus, it is so bleak [to see] the use of the black velvet patch for the face, a bump on the temple, a sign of bone lacking in the forehead, that one no longer dares to look; so that if we were to meticulously ponder, and notice the broken color [of the face], the little pains in the joints, the small blisters and sores around the mouth . . . we could go on forever; but at last we are able to cleanly extract our proposition, which is the certain and well examined conclusion, that there is no other province or kingdom in the world where this disease afflicts more, nor where more mercury, guaiacum, china, and sarsaparilla are consumed . . .81
43The reference to bumps, blisters, and pains in the joints are just some of the more common symptoms that were recorded by chroniclers in the sixteenth century. The surgeon Arias describes the signs of morbo gálico as sores on the penis, swellings in the groin area, pains in the joints, the loss of hair, especially the eyebrows and eyelashes, sores in the mouth, bad digestion, headaches without fever, bumps on the head, very bad color in the face, and "weakness, such that they are too tired to walk and desire to sit and do not want to get up again."82 Bernal Díaz tells us that many of Cortés's soldiers had trouble descending the steep stairs of the Aztec temple in Tenochtitlan because "they were suffering from bubas or humors, and it hurt their muscles to walk down."83 The name bubas comes from the distinctive sores and swellings that appear on all parts of the body, including the skin of the palms and soles, and in the mouth as well as around the genitalia and the anus. Today, we know that these symptoms are characteristic of secondary syphilis, which sets in about six weeks after the primary sore, or chancre, appears on the genitals. After the secondary symptoms heal and disappear, there is a latent period, which can last many years, during which time the treponemes that cause the disease lurk in the tissues and intermittently in the blood and spinal fluid. During this time, the sufferer may be free of symptoms. Late, or tertiary, syphilis displays itself with the onset of more serious, even life-threatening, complications: the destruction of bone; inflammation of the heart and blood vessels, the eyes, or central nervous system; and lastly, syphilis can attack the brain itself, creating extreme dementia, even insanity.84 That this dreadful disease revealed itself in three different stages was not known until the middle of the nineteenth century when the French venereologist, Philippe Ricord, described the natural progression of the illness.85
44The variety of symptoms described by observers and sufferers in its early days underscores the need to be cautious about drawing too rigid a picture of the disease, which clearly changed over the years. In its first decades of existence, there is evidence that the malady was quite malignant and deadly. Like any infectious disease that is introduced into a population with little or no immunity, the classic course of the illness is rapid spread and extreme virulence, followed later by diminishing severity. Descriptions of the malady from the late fifteenth and early sixteenth centuries relate the horror of its effects: the terrible sores and swellings, often extending into the mouth and throat, and leaving the body covered with scabs that turned from red to black; severe fever; pain in the bones so intense that patients "screamed day and night without respite, envying the dead themselves"; and, often early death. By the seventeenth century, however, syphilis had likely become the disease we know it to be today: a very dangerous infection, but not one that would "be called explosive in the nature of its attack on the victim."86 It is also important to remember that bubas was sometimes used as a catch-all term to denote a wide collection of symptoms. Syphilis, in some of its dermatologic manifestations, resembles leprosy; and, as Esteyneffer notes, bubas and scurvy are sometimes confused because their pains in the joints and bones are similar. Furthermore, individuals could be infected with more than one disease, or more than one venereal disease, at a time, accounting for a sometimes bewildering mixture of physical symptoms. Given these circumstances, it would be difficult for even a sophisticated diagnostician to make an accurate inference about the identity and natural course of the illness.87
45The historiography of syphilis is vast and its origins have been debated since its first appearance in Western Europe in the last decade of the fifteenth century. Alfred Crosby has noted the special fascination this illness holds for historians, which he attributes to its abrupt beginnings:
. . . of all mankind's most important maladies, it is the most uniquely "historical." The beginnings of most diseases lie beyond man's earliest rememberings. Syphilis, on the other hand, has a beginning. Many men, since the last decade of the fifteenth century, have insisted that they knew almost exactly when syphilis appeared on the world stage and even where it came from.88
46Among the early chroniclers of the disease, there is a broad consensus that it first appeared in Italy sometime between the years 1494–6 when King Charles VII of France led an attack against the Kingdom of Naples. His army was made up of about 30,000 men—mostly mercenaries, including some from Spain—and, like most armies of the day, was accompanied by an assortment of civilians, including hundreds of prostitutes. When the invaders were finally ejected by King Alphonso II with the help of Spanish mercenaries sent by Ferdinand and Isabella, they continued to spread the disease far and wide as they returned to their own countries. Charles himself died of syphilis in 1498. By this time, with the disease raging throughout continental Europe, it was estimated that about 20 percent of the population was infected with what was now being called the French disease.89
47Controversy about whether syphilis existed in the Old World before the return of Columbus from the New World has continued from the early sixteenth century to our own time. The vast accumulation of documentary materials and, since the late nineteenth century, new evidence from the evolving field of paleopathology has had the effect of extending, rather than settling, the debate. Although proponents of an American origin for the disease cite some persuasive evidence to back up their theory, a large part of their argument rests on the conspicuous lack of evidence that syphilis ever existed anywhere on the Eurasian continent: first, no unequivocal description of it has ever been found in written sources predating the late fifteenth century, none, that is, that would clearly distinguish it from diseases with similar symptoms such as leprosy or scabies, a fact hard to ignore for a disease that spreads as widely and as quickly as syphilis does wherever people are exposed to it; and, second, no human remains dating from before the 1490s showing signs of syphilitic damage have ever been found in the countless excavations of Old World civilizations. This striking absence of any sign of Old World origins is bolstered by some documentary evidence from the early years of the Spanish empire and a steadily growing collection of physical evidence indicating American provenance. Nearly a generation after the Colombian voyages, medical men and historians began insisting that the new disease was brought back to Europe by Columbus's crew in 1493. Both Bartolomé de las Casas and Gonzalo Fernández de Oviedo y Valdés, two of the most important early chroniclers of Spanish America, and each with personal experience and access to people who sailed with Columbus, argued that the disease was clearly imported into Europe by the first voyagers to return from the New World. Their claim was backed up by others, including Columbus's son, Ferdinand, and a Spanish physician named Ruy Díaz de Isla who claimed that he had treated some of the sailors for an unknown disease whose symptoms later turned out to be those of morbo gálico. Even more persuasive then such claims are the growing number of physical remains excavated from American soil. Precontact skeletons showing syphilitic damage have been identified by paleopathologists, bolstering the argument that treponemal diseases, including syphilis, existed in New World populations. Another theory complicating this debate is one that holds that treponemal diseases had long been present in the Old World prior to the epidemic, although not in the form of a venereal disease. Changes in social and environmental conditions triggered a change in symptoms and modes of transmission; the social and political disruptions of late-fifteenth-century Europe—widespread warfare, increased travel, changing sexual norms—account for the sudden and dramatic nature of the epidemic. The dispute about the origins of syphilis is unlikely to be settled any time soon, and, in any event, it is not my intention here to revisit this debate. What is clear, however, is that for Europeans living at the turn of the sixteenth century, syphilis constituted something new and horrifying.90
48Perhaps a more relevant question for our purposes is: how did early modern Europeans themselves make sense of the sudden appearance of this horrible malady? The variety of names given the new disease offers an important clue. At stake in determining the origins of the disease, especially in one transmitted sexually, is the desire to attribute responsibility to a group other than one's own. New and bad diseases come from somewhere else, brought by people with bad habits. Thus, the Italians called it the French disease, a name that endured despite efforts by the French, who preferred to call it the disease of Naples. But nothing was so distant, foreign, and unknown than the New World and to many it came to seem natural that the new disease should have come from there. Not only did the sudden appearance of the French disease in Europe coincide with Columbus's voyages, but also one of the most popular early remedies came from America. A predominant belief of the day was that God always provided a corresponding cure in the same place that He inflicts a disease. This was guaiacum, sometimes called palo santo, a wood from a tree native to the West Indies. The wood was broken into very small pieces and boiled in water resulting in a decoction that was used both as a topical and internal medicine. Holy Wood's reputed miraculous effects were widely praised by patient and practitioners alike, and during the 1520s its use was adopted all over Europe. The treatment caused the patient to sweat profusely, a desirable effect according to humoral theory, as this rid the body of its impurities. Apart from its American provenance, guaiacum's popularity may also have been aided by its relatively mild side effects, especially when compared to the other standard treatment of the day, mercury, which caused horrendous suffering in its recipients. Although the topical and internal use of this drug was the only relatively effective means of treating syphilis for the next four hundred years, its overuse killed many patients by poisoning them.
^topAchaques y indisposiciones: Everyday Ailments
49Colonial documents suggest that an even broader experience of illness was formed by the less life-threatening physical ailments that tend to be overlooked by the historian. Minor maladies and discomforts—conditions that are routinely and successfully treated today—afflicted everyone and added to the general anxiety about health. Because contemporary conceptions of disease emphasized symptomology, people recognized that even minor symptoms could initiate a major decline. Health, as we will see later, was the product of a carefully preserved balance, not a state of permanency, thus the individual had every reason for closely observing changes in routine bodily functions and on the outer surfaces of the body. It is not surprising, then, that the concern with everyday health meant keeping a close watch on both the body's evacuations and cutaneous manifestations that now might be regarded as superficial.91 Maladies that manifested themselves on the skin were one of the most common categories of everyday disorders; the manuals of domestic medicine are full of treatment advice for the boils, ulcers, sores, tumors, and swellings that afflicted everyone. Today, within the hierarchy of modern medicine, skin conditions are not considered serious threats to health, but in past centuries this was, in both theory and practice, a major area of concern.
50An anonymous observer in sixteenth-century New Spain wrote that "the ordinary diseases of the Spanish are apostems from which they die."92 As with fevers, these apostemas, or fluid-filled swellings, are another example of how early moderns named and treated symptoms as disease entities. And like fevers, too, apostems were a rather large and general diagnostic category. The surgeon Alonso López de Hinojosos, who wrote a practical handbook on surgery for the nonprofessional in 1578, devoted twenty-seven chapters to the various types of apostemas. Here he describes a bewildering variety of maladies from which people suffered: gangrene of the limbs or digits; carbuncles; lamparones (painful swellings of the neck); empeines (a pustular skin rash); encordios (swellings of the groin area); sarna, or scabies; and an infinite diversity of growths, bumps, and protuberances which tend to appear anywhere on the head, eyes, nostrils, ears, or on the breasts.93 At one point during his travels through New Spain, Fray Alonoso Ponce was much indisposed by an apostem of his right nipple, which:
. . . was growing each day and getting worse . . . and even though they made him many benefactions and they applied a thousand remedies, none of them helped, until they gave him a piedra cornerina [a type of stone], which had the virtue, once placed on the swelling, of sticking to the meat and sucking out, bit by bit, the bad humor and softening it and reducing the swelling a great deal . . .
Unfortunately, the padre comisario's apostema returned, along with other "achaques e indisposiciones" ("ailments and indispositions"), causing him several more months of agony.94
51
 Anonymous ex-voto, 18th-century, Mexico.
The continuous narration of miraculous cures that circulated through colonial Mexico contains an abundance of sufferers' testimony relating their experience with these kinds of ailments. Many examples can be found in painted ex-votos from the eighteenth century. The young child of Juan Pavón, a sacristan in Mexico City, was alleviated of "apostema in the throat" when he was anointed with lamp oil from the Virgin of Guadalupe's shrine. Don Juan de Peñafiel, a king's official, "desperate from lamparones and empeines," was cured when his skin was rubbed with the sacred dirt from the sanctuary of San Miguel. A young woman's illness produced "interior sores (llagas ynteriores) on the whole of her back so that she could not be in bed, seated or standing"; the pain was so severe it penetrated right through her "bones, nerves, and entrails, [so that] she was just waiting to die." Happily for this doncella, her suffering came to an end "after 19
Anonymous ex-voto, 18th-century, Mexico.
The continuous narration of miraculous cures that circulated through colonial Mexico contains an abundance of sufferers' testimony relating their experience with these kinds of ailments. Many examples can be found in painted ex-votos from the eighteenth century. The young child of Juan Pavón, a sacristan in Mexico City, was alleviated of "apostema in the throat" when he was anointed with lamp oil from the Virgin of Guadalupe's shrine. Don Juan de Peñafiel, a king's official, "desperate from lamparones and empeines," was cured when his skin was rubbed with the sacred dirt from the sanctuary of San Miguel. A young woman's illness produced "interior sores (llagas ynteriores) on the whole of her back so that she could not be in bed, seated or standing"; the pain was so severe it penetrated right through her "bones, nerves, and entrails, [so that] she was just waiting to die." Happily for this doncella, her suffering came to an end "after 19  Ex-voto to the Virgin of Soledad.
days, without any remedy other than the image (estampa) of [San Miguel] that she had placed on her back." And, finally, there is the case of little Hipólito, the infant son of Spanish parents living in the city of Oaxaca, whose illness of "two apostemas right under the arms" required such extensive bandaging and binding that he "could not move for two days." The supplications to La Soledad, the patron saint of the city, were successful, but because the parents were slow in fulfilling their vow to commission the ex-voto, Hipólito suffered a relapse of "many symptoms [accidentes] all of them very mortal."95 Apparently, the disease category of apostema was not limited to ailments that manifested themselves only on the surface of the body; internal organs were affected by apostems, too. A sixteenth-century resident of Mexico City writes to his wife in Seville about his desperate state of health: ". . . since coming here I have not had one day of health, and all of the month of July and August I was in bed, and without any hope, so that the doctors wanted to open me up, because they said that my disease was an apostem on my liver . . ." This letter-writer eventually got better—without surgery, luckily—but only after much bleeding and purging.96
Ex-voto to the Virgin of Soledad.
days, without any remedy other than the image (estampa) of [San Miguel] that she had placed on her back." And, finally, there is the case of little Hipólito, the infant son of Spanish parents living in the city of Oaxaca, whose illness of "two apostemas right under the arms" required such extensive bandaging and binding that he "could not move for two days." The supplications to La Soledad, the patron saint of the city, were successful, but because the parents were slow in fulfilling their vow to commission the ex-voto, Hipólito suffered a relapse of "many symptoms [accidentes] all of them very mortal."95 Apparently, the disease category of apostema was not limited to ailments that manifested themselves only on the surface of the body; internal organs were affected by apostems, too. A sixteenth-century resident of Mexico City writes to his wife in Seville about his desperate state of health: ". . . since coming here I have not had one day of health, and all of the month of July and August I was in bed, and without any hope, so that the doctors wanted to open me up, because they said that my disease was an apostem on my liver . . ." This letter-writer eventually got better—without surgery, luckily—but only after much bleeding and purging.96
52Also prevalent and, judging from the bewildering variety of remedies offered to contemporaries, of crucial concern, was a whole host of conditions that were associated with urination, including the dreaded kidney stone. Afflictions associated with urination were a very common health problem. Contemporaries simply called this condition mal de orina, or disease of the urine, but the domestic medicine guides give some idea what this meant for the sufferer. Both Gregorio López and Esteyneffer describe these various problems as urine with blood, urine with rotten material, urination with pain, urination without sensation (incontinence), and inability to urinate. The infinite number of remedies for mal de orina also suggests that many people sought relief from these types of symptoms. Treatments ranged from the usual bleeding and purgings and the use of ordinary herbs and foods—achiote in chocolate, rose mallow, clover, sheep's milk, and recently laid chicken eggs—to more bizarre ingredients. López, for example, suggests that horse manure cooked in wine and placed hot on the patient's navel will help with blood in the urine; likewise, the sufferer of orina podrida, or urine with foul material, can be cured by drinking a mixture of rabbit's urine and pulque blanco.97
53But surely the most dreaded malady associated with the urinary tract was la piedra, the kidney or bladder stone, a very common illness until the nineteenth century. Renal stones develop when abnormal concretions of calculi form in the kidneys or bladder, becoming impacted and sometimes obstructing the flow of urine. This condition, although not usually life-threatening, can cause its victim extreme discomfort and pain as the stones travel through the urinary tract. Stones originating in the bladder are rare today in industrialized countries, although they were quite common in earlier centuries; stones originating in the kidneys—"kidney stones"—today still affect about 5 percent of the population.98 Poor nutrition and lack of variation in the diet—something that occurred at all levels of society—probably contributed to the prevalence of this condition in New Spain, as it did in Western Europe. That renal stones were a frequent health problem for many people is evident from the frequent references made to a vast assortment of remedies and practitioners that specialized in treating this malady. One study of Spanish medicine in the sixteenth and seventeenth centuries has identified a large group of practitioners whose activities were watched and debated in the Acts of the Castilian Court. These empirics were described as being proficient in the "art of extracting stones from the bladder and demolishing and curing those of the kidneys and curing growths and all pains of the urine (pasiones de orina), in men as well as women, without recourse to cutting with instruments (hierros), [in] boys and girls, and other aliments and illnesses that men tend to get in the scrotum and hidden parts . . ." The demand for these services must have been high as the royal authorities granted permission to many of these practitioners to teach their skills to others.99
54Kidney stones were generally treated with medicines but sometimes more aggressive means were used to extract them. A doctor practicing in Mexico in the mid-sixteenth century witnessed an operation in which a stone "the size of an egg" was removed from a patient.100 Lithotomy, the surgical removal of the stone, had been practiced from the first century AD by a method known as the "apparatus minor": a finger in the rectum forced the stone to bulge into the perineum, making it possible to cut and remove it without the use of other instruments. Early in the sixteenth century, a new method was widely adopted. Called the "apparatus major," it involved dilating and incising the urethra just in front of the bladder neck to allow the introduction of several instruments to extract the stone. This technique—which, in an age before anesthesia, must have been an excruciating experience for the patient—avoided damage to the prostate gland and seminal vesicles, which commonly led to excessive bleeding and even incontinence after the older technique. In the eighteenth century, new methods of stone extraction were developed and many surgeons promoted their own variations and instrumentation. Lithotomy, which had been practiced almost exclusively by unlicensed practitioners in the sixteenth century, was gradually appropriated by licensed surgeons by the end of the eighteenth.101
55Eye disorders also were widespread, and of all the senses, the threat to sight caused the most anxiety. On one occasion, when her daughter was suffering from an eye inflammation, the Condesa de Miravalle sent mesquite wood, a common remedy for mal de ojos. Cataracts, or nubes en los ojos, were a common condition, the cause of which was usually attributed to the environment. According to compilers of the Relaciones Geográficas the Indians of Quautlatlauca suffered from them because they lived in a land that was "very white and dry," as did the residents of Tecpamatitlan, where the fog was so thick that "one can not see the houses, and besides causing sadness and melancholy, this is very damaging for the eyes, as many Indians in this village have cataracts."102
56Another troublesome affliction was toothache. The surgeon López de Hinojosos's first piece of advice for this malady was "never let the barber pull a tooth until he has tried some remedies for the pain, like vinegar cooked with some pepper corns."103 Tooth-pulling, performed by a barber-surgeon, or perhaps a more specialized sacamuelas, or "toothpuller," was almost always the treatment of last resort in an age before modern dentistry was able to treat tooth decay effectively. This does not mean, however, that people of past centuries did not pay attention to their dental health; in fact, lots of historical sources strongly indicate the contrary. Not only were they concerned with what to do about cavities, loose teeth, bleeding gums, abscesses, and, most important, ending the incessant pain of a decayed tooth, but they worried as well about how their teeth looked and breath smelled.104 La Gaceta de México, a newspaper published in the later colonial years, is full of advertisements such as this one offering a "dental elixir which is very useful for the fluxuations and pains of the molars and teeth, roots and gums, it secures teeth firmly in place, gets rid of filth and tartar, and prevents scurvy and bad breath . . ." Included in the price of 10 reales was the exlir's own recipe, so one could reproduce the remedy at home.105
57
 Ex-voto to Our Lady of Tulantongo.
This exploration of everyday ailments could go on indefinitely. Even a casual glance at the remedies in circulation during the colonial period reveals a whole variety of other commonly endured conditions such as hernia, constipation, hemorrhoids, sciatica, rheumatism, and gout. In addition to these, women suffered from the usual menstrual problems, difficult pregnancies, dangerous deliveries, puerperal fever, mal de madre, and complications with breastfeeding. The ex-voto of Maria Narajo, painted in 1774, expresses, both pictorially and with text, the risky business that was childbirth at this time. ". . . around 9 in the evening Maria Naranjo began to have pains of childbirth and at dawn the next morning they had to remove the child by hand; the paturient continued to suffer with great risk to her life until [the next day]." Earnest appeals were made by the family and midwife to Nuesta Señora de Tulantongo, to whom the ex-voto is dedicated.106 Nor can we overlook the early modern preoccupation with mood and state of mind. In his chapter on melancholia, Farfán notes that this surprisingly common disease afflicts and torments many, and that men and women scarcely reach the age of twenty when they begin to complain of it. Some of the symptoms include generalized "fears and frights," abnormal fears of death, insomnia, lack of appetite, and a "tightening of the throat and a feeling like one is being drowned," the latter that sounds very much like the "panic attack" of today. True to his Galenic training, Farfán explained this disease in terms of physical factors. One form of melancholia arises from "sediments" of the blood, and is cold and dry, whereas another originates in the liver and "burns with excessive heat."107 The Condesa de Miravalle's chronically ailing daughter, Maria Antonia, appears to have suffered greatly from this disorder. In one letter the mother warns her daughter to be mindful of her moods "because from these melancolicas come many bad things."108
Ex-voto to Our Lady of Tulantongo.
This exploration of everyday ailments could go on indefinitely. Even a casual glance at the remedies in circulation during the colonial period reveals a whole variety of other commonly endured conditions such as hernia, constipation, hemorrhoids, sciatica, rheumatism, and gout. In addition to these, women suffered from the usual menstrual problems, difficult pregnancies, dangerous deliveries, puerperal fever, mal de madre, and complications with breastfeeding. The ex-voto of Maria Narajo, painted in 1774, expresses, both pictorially and with text, the risky business that was childbirth at this time. ". . . around 9 in the evening Maria Naranjo began to have pains of childbirth and at dawn the next morning they had to remove the child by hand; the paturient continued to suffer with great risk to her life until [the next day]." Earnest appeals were made by the family and midwife to Nuesta Señora de Tulantongo, to whom the ex-voto is dedicated.106 Nor can we overlook the early modern preoccupation with mood and state of mind. In his chapter on melancholia, Farfán notes that this surprisingly common disease afflicts and torments many, and that men and women scarcely reach the age of twenty when they begin to complain of it. Some of the symptoms include generalized "fears and frights," abnormal fears of death, insomnia, lack of appetite, and a "tightening of the throat and a feeling like one is being drowned," the latter that sounds very much like the "panic attack" of today. True to his Galenic training, Farfán explained this disease in terms of physical factors. One form of melancholia arises from "sediments" of the blood, and is cold and dry, whereas another originates in the liver and "burns with excessive heat."107 The Condesa de Miravalle's chronically ailing daughter, Maria Antonia, appears to have suffered greatly from this disorder. In one letter the mother warns her daughter to be mindful of her moods "because from these melancolicas come many bad things."108
58
 Ex-voto to the Virgin of Soledad.
And, finally, to these endemic and chronic illnesses must be added the dangers of everyday life. Falls from buildings and scaffolding, fires, drownings, mishaps with tools, overturned carriages, falls and kicks from horses and mules, and encounters with bandits were just some of the hazards people encountered. The personal testimonies in the form of ex-votos left by survivors of these accidents provide one of the best windows we have to view this side of life. A man is thrown from his mule and has trouble getting clear of the bucking animal; another is attacked by thieves on the road to his house, stabbed in the side, and left for dead. A third, as shown in this ex-voto from the eighteenth century, takes a bad fall while he is collecting corn from a storage area on a rooftop.109 In these personal testimonies from the eighteenth century, the victims miraculously survived their ordeals. But in an age without adequate emergency services, the trauma from accidents and violence must have been especially feared as blood loss could quickly kill. The maintenance of health and the relief of anxiety about health thus created a high demand for all kinds of medical advice and care.
Ex-voto to the Virgin of Soledad.
And, finally, to these endemic and chronic illnesses must be added the dangers of everyday life. Falls from buildings and scaffolding, fires, drownings, mishaps with tools, overturned carriages, falls and kicks from horses and mules, and encounters with bandits were just some of the hazards people encountered. The personal testimonies in the form of ex-votos left by survivors of these accidents provide one of the best windows we have to view this side of life. A man is thrown from his mule and has trouble getting clear of the bucking animal; another is attacked by thieves on the road to his house, stabbed in the side, and left for dead. A third, as shown in this ex-voto from the eighteenth century, takes a bad fall while he is collecting corn from a storage area on a rooftop.109 In these personal testimonies from the eighteenth century, the victims miraculously survived their ordeals. But in an age without adequate emergency services, the trauma from accidents and violence must have been especially feared as blood loss could quickly kill. The maintenance of health and the relief of anxiety about health thus created a high demand for all kinds of medical advice and care.
Notes
Note 1: Jared Diamond, Guns, Germs, and Steel: The Fates of Human Societies (New York: W.W. Norton & Co., 1999). back
Note 2: Robert McCaa, "The Peopling of Mexico from Origins to Revolution," in A Population History of North America, ed. Michael R. Haines and Richard H. Steckel (Cambridge: Cambridge University Press, 2000) pp. 248–9; Rebecca Storey, Life and Death in the Ancient City of Teotihuacan: A Modern Paleodemographic Synthesis (Tuscaloosa: University of Alabama Press, 1992), p. 237. back
Note 3: Sherburn Cook, "The Incidence and Significance of Disease among the Aztecs and Related Tribes," The Hispanic American Historical Review, 26 (1946), 332; Carlos Viesca T. "Hambruna y epidemia en Anáhuac (1450–1454) en la época de Moctezuma Illhuicamina," in Ensayos sobre la historia de las epidemias en México, ed. Enrique Florescano and Elsa Malvido (México: Instituto Méxicano del Seguro Social, 1982), p. 163. back
Note 4: Marshall T. Newman, "Aboriginal New World Epidemilogy and Medical Care, and the Impact of Old World Disease Imports," Physical Anthropology, 45:3 (November 1976), 667–72; Lourdes Márques Morfín, et al., "Health and Nutrition in Prehispanic Mesoamerica," in The Backbone of History: Health and Nutrition in the Western Hemisphere, ed. Richard H. Steckel and Jerome C. Rose (Cambridge University Press, 2002); Robert McCaa, "The Peopling of Mexico"; Rebecca Storey, Life and Death in the Ancient City of Teotihuacan; Lourdes Márqiez Morfín, et al., Playa del Carmen: Una población de la costa oriental en el postclásico (un estudio osteológico) (México: Instituto Nacional de Antropología e Historia, 1982). back
Note 5: Storey, p. 18; Douglas H. Ubelaker, "Patterns of Disease in Early North American Populations," in Haines and Steckel, p. 55. back
Note 6: Mark Nathan Cohen, Health and the Rise of Civilization (New Haven, CT: Yale University Press, 1989); T. Aiden Cockburn, "Infectious Disease in Ancient Populations," Current Anthropology, 12 (1971), 45–66. back
Note 7: Márquez Morfín, et al., "Health and Nutrition," p. 15; Storey, p. 231. back
Note 8: Storey, p. 257. back
Note 9: MaCaa, "The Peopling of Mexico," pp. 246–7. back
Note 10: Márquez Morfín, et al., "Health and Nurtrition," pp. 20–1; on tortilla making and women, see Arnold Bauer, "Millers and Grinders: Technology and Household Economy in Meso-America," Agricultural History, 64:1 (Winter 1990), 1–17. back
Note 11: Márques Morfín, et al., "Health and Nutrition," p. 23. back
Note 12: Ubelaker, pp. 57–63; MaCaa, "The Peopling of Mexico," p. 246. back
Note 13: Fray Bernardino de Sahagún, Florentine Codex, General History of the Things of New Spain, ed. and trans. C. E. Dibble and A. J. O. Anderson, 12 books (Salt Lake City: University of Utah Press, 1950–69), I:31, XI:173; Bernard R. Ortiz de Montellano, Aztec Medicine, Health, and Nutrition (New Brunswick, NJ: Rutgers University Press, 1990), p. 120. back
Note 14: Newman, p. 669; Cook, "Disease among the Aztecs," pp. 325–7. back
Note 15: Alfred Crosby Jr., The Colombian Exchange: Biological and Cultural Consequences of 1442 (Westport, CT: Greenwood Press, 1972), p. 37. back
Note 16: Margaret Pelling, The Common Lot: Sickness, Medical Occupations and the Urban Poor in Early Modern England (London: Longman, 1998), p. 28. back
Note 17: Zaida M. Feliciano, "Mexico's Demographic Transformation: 1920 to 1990," in Haines and Steckel, p. 608. back
Note 18: Kenneth F. Kiple, "The Ecology of Disease," in Companion Encyclopedia of the History of Medicine, 2 vols., ed. W. F. Bynum and Roy Porter (London: Routledge, 1993), Vol. I, pp. 375–7, hereafter cited as CEHM. back
Note 19: Diamond, p. 210. back
Note 20: Enrique Florescano and Elsa Malvido, Ensayos sobre la historia de las epidemias México; Alfed W. Crosby Jr., "Conquistador y pestilencia: The First New World Pandemic and the Fall of the Great Indian Empires," HAHR, 47 (1967), 321–37; Alfred W. Crosby Jr., The Columbian Exchange: Biological and Cultural Consequences of 1492; Robert McCaa, "Spanish and Nahuatl Views on Smallpox and Demographic Catastrophe in Mexico," Journal of Interdisciplinary History, XXV:3 (Winter 1995), 397–431; Noble David Cook and W. George Lovell, Secret Judgements of God: Old World Disease in Colonial Spanish America (Norman: University of Oklahoma Press, 1991); Thomas M. Whitmore, Disease and Death in Early Colonial Mexico: Simulating Amerindian Depopulation (Boulder, CO: Westview Press, 1992). back
Note 21: Cook and Lovell, "Unraveling the Web of Disease," in Secret Judgements of God, p. 216; Sherburne F. Cook and Woodrow Borah, The Indian Population of Central Mexico, 1531–1610, Ibero-Americana, 44 (Berkeley and Los Angeles, 1960); Shelburn F. Cook and Woodrow Borah, Essays in Population History, 3 vols. (Berkeley and Los Angeles: University of California Press, 1971–9). back
Note 22: Whitmore, pp. 109–20. back
Note 23: Charles Gibson, The Aztecs under Spanish Rule: A History of the Indians of the Valley of Mexico, 1519–1810 (Stanford: Stanford University Press, 1964), pp. 448–9; Peter Gerhard, A Guide to the Historical Geography of New Spain, rev. ed. (Norman: University of Oklahoma Press, 1993), p. 23. back
Note 24: Anthony Pagden, ed. and trans., Hernán Cortés: Letters from Mexico (New Haven, CT: Yale University Press, 1986), pp. 164–5; Bernal Diaz del Castillo, Historia verdadera de la conquista de la Nueva España (México: Alianza Editorial, 1991), p. 416; Anals de Tenochtitlan (Codex Aubin) in We People Here: Nahuatl Accounts of the Conquest of Mexico, ed. and trans. James Lockhart (Berkeley: University of California Press, 1993), p. 279. back
Note 25: Book Twelve of The Florentine Codex, in Lockhart, We People Here, pp. 181–5. back
Note 26: Crosby, The Columbian Exchange, p. 46; Cecil Textbook of Medicine, 19th ed., ed. James B. Wyngaarden, M.D., Lloyd H. Smith Jr., M.D., and J. Claude Bennett, M.D. (Philadelphia: W.B. Saunders Company, 1992), pp. 1842–3; Lovell and Cook, "Unraveling the Web of Disease," p. 218; Richard Preston, "The Demon in the Freezer: How Smallpox, A Disease Officially Eradicated Twenty Years Ago, became the Biggest Threat We Now Face," The New Yorker, July 12, 1999, pp. 44–64. back
Note 27: Toribio de Benavente o Motolinía, Memoriales o libro de las cosas de la Nueva España y de los naturales de ella, ed. Edmundo O'Gorman (México: UNAM, 1971), p. 21; Licenciado Lucas Vásquez de Ayllón, "Relación que hizo el Licenciado Lucas Vásquez de Ayllón, de sus diligencias para estorbar el rompiemiento entre Cortés y Narváez," in Cartas y relaciones de Hernán Cortés al Emperador Carlos V, ed. Pascual de Gayango (Paris, 1866), p. 42, quoted in McCaa, "Spanish and Nahuatl Views on Smallpox," p. 432. back
Note 28: Crosby, Ecological Imperialism: The Biological Expansion of Europe, 900–1900, (Cambridge: Cambridge University Press, 1986), p. 286; Hanns J. Prem, "Disease Outbreaks in Central Mexico during the Sixteenth Century," in Cook and Lovell, p. 25. back
Note 29: Kiple, pp. 368–9; Crosby, Ecological Imperialism, p. 34. back
Note 30: Kiple, pp. 358–9; Diamond, pp. 203–5. back
Note 31: Diamond, pp. 202–3. back
Note 32: Ibid., pp. 212–13; Crosby, Ecological Imperialism, pp. 30–1. back
Note 33: Diamond, p. 213. back
Note 34: Motolinía, p. 413; "Carta del virey de la Nueva España, Don Martín Enriquez al Rey Don Felipe II," in Cartas de Indias (Madrid, 1877), Vol. I, p. 331; "Carta de Fray Domingo de Betanzos," in Colección de documentos para la historia de México, ed. Joaquín García Icazbalceta (México, 1866), p. 200; Diego Muñoz Camargo, "Descripción de la ciudad y provincia de Tlaxcala," in Relaciones Geográficas del siglo XVI: Tlaxcacla, ed. René Acuña, 10 vols. (Méxcio: UNAM, 1984), Vol. V., pp. 75–6, hereafter cited as RG. back
Note 35: Sahagún, cited in German Somolinos d'Ardpos, "Las epidemias en México durante el siglo XVI," Florescano and Malvido, p. 208. back
Note 36: Eloise Quiñones Keber, Codex Tellerianso-Remensis: Rituals, Divination, and History in a Pictorial Aztec Manuscript (Austin: University of Texas Press, 1995), Folio 46v, pp. 96 and 238. back
Note 37: Papeles de Nueva España publicados de orden y con fondos del gobierno mexicano por Francisco del Paso y Troncoso, 2a serie, Geográfica y Estadística (México: Editoral Cosmos, 1979): Relación de Cuauhquilpan, p. 307; Relación de Huezutla, p. 185; Relación de Mexicalzinco, p. 195: Relación de Ocopetlayuca, p. 258; Relación de Atitalaquia, p. 202, hereafter cited as PNE. back
Note 38: Ciudad Real, Antonio de, Tratado curioso y docto de las grandezas de la Nueva España, (México: Instituto de Investigaciones Históricas, UNAM, 1993) Vol. II, p.131. back
Note 39: Motolinía, p. 21. back
Note 40: "Juan López de Soria a la condesa de Ribadavia," México: November 30, 1576, in Enrique Otte, editor, Cartas Privadas de Emigrantes a Indias, 1540–1616 (México: Fondo de Cultura Económica, 1993), pp. 96–7. back
Note 41: Hans Zinsser, Rats, Lice, and History, (Boston: Atlantic Monthly Press, 1963) p. 120; Whitmore, p. 54. back
Note 42: Cited in Gibson, p. 449. back
Note 43: Prem, p. 33. back
Note 44: Fray Gerónimo de Mendieta, Historia Eclesiástica Indiana (México: Editorial Salvador Chavez Hayhoe, 1945), Vol. III, p.174. back
Note 45: Códice de 1576, cited in Somolinos, 1982, pp. 212–13. back
Note 46: PNE: "Relación de Ocopetlayuca," p. 258; Gerhard, p. 329. back
Note 47: Francisco Javier Alegre, Historia de la Compania de Jesús en Nueva España, ed. Carlos María Bustamante (México, 1841–2), Vol. II, p. 262; see also Cayetano de Cabrerra y Quintero, Escudo de Armas de México (México: Instituto Mexicano del Seguro Social, 1981); América Molina del Villar, La Nueva España y el matlazahuatl, 1736–1739 (México: Centro de Investigaciones y Estudios Superiores en Antropología Social/El Colegio de Michoacán, A.C., 2001). back
Note 48: Zinsser, pp. 216–64; Nicholás León, "Qué era el Matlazáhuatl y qué el Cocoliztli en los tiempos precolumbinos y en la época hispana?" in Florescano and Malvino, Vol. II, p. 383; Cook and Lovell, "Unraveling the Web of Disease," pp. 225–7. back
Note 49: Francisco de las Barras y Aragón, "Viaje del astrónomo francés Chappe a California en 1796, y noticias de J. A. Alzate sobre la historia natural de Nueva España,"Anuario de estudios americanos, Vol. I (1944), p. 767, cited in Donald B. Cooper, Epidemic Disease in Mexico City, 1761–1813: An Administrative, Social, and Medical Study (Austin: University of Texas Press, 1965), p. 49. back
Note 50: Cooper, p. 54. back
Note 51: Ex-voto to Our Lady of Sorrows and to San Sebastian. Anonymous, 1761. Franz Mayer Museum, Mexico City. back
Note 52: Archivo Manuel Romero de Terreros (Pachuca, Mexico): Miravalles, 23 de Mayo, 1762; 27 de enero, 1763; and 12 de noviembree, 1761, hereafter cited as AMRT. back
Note 53: Elsa Malvido, "Cronología de epidemias y crisis agrícolas en la época colonial," and "Efectos de las epidemias y hambrunas en la población de México (1519–1810)," in Florescano and Malvido, pp. 171–8, 179–200. back
Note 54: Cabrera y Quintero, pp. 67–71; Gibson, pp. 448–51; MaCaa, "The Peopling of Mexico," p. 260. back
Note 55: MaCaa, "The Peopling of Mexico," p. 260. back
Note 56: Ciudad Real, Vol. I, p. 149; RG, I: 30, V: 38, 74 346, 408, VI: 79, 88, 302; PNE, pp. 10, 76, 91, 103, 120, 287; AMRT, Miravalles, 2 de julio de 1757. back
Note 57: Juan de Cárdenas, Primera parte de los problemas y secretos maravillosos de las Indias (Madrid: Alianza Editorial, 1988), pp. 240–1. back
Note 58: Fray Agustín Farfán, Tractado breve de medicina, facs. ed. (Madrid: Ediciones Culturas Hispanica, 1944), pp. 1–2. back
Note 59: Ibid., p. 2. back
Note 60: "Alonso de Alcocer a su hermano Juan de Colonia, en Madrid," México: 10 de diciembre, 1577; "Gaspar de Vargas a Alonso Pérez Pocasangre, in Jaén," México: 5 de noviembre, 1564; "Maria Diaz a su hija Inés Díaz, en Sevilla,"México: 31.de marzo, 1577, in Otte, pp. 98–9, 45, 97–8. back
Note 61: Farfán, pp. 9–10; Esteyneffer, pp. 272–3. back
Note 62: "Juan de Brihuega a su hermano Pedro Garcia, en Briguega," Puebla: 16 de enero, 1572, in Otte, p. 154. back
Note 63: RG, II: 154, 168. back
Note 64: "Marcos Ortiz a su padre," México: 22 de febrero, 1569, in Otte, p.54; Ciudad Real, I. p. 26. back
Note 65: Lenard G. Wilson, "Fevers," in CEHM, pp. 384–5. back
Note 66: Cook, "Disease among the Aztecs and Related Tribes," p. 323; Ortiz de Montellano, p, 122. back
Note 67: Miguel E. Bustamante, "La fiebre amarilla en México y su origen en América," in Florescano and Malvido, p. 27; Andrew L. Knaut. "Yellow Fever and the Late Colonial Public Health Response in the Port of Veracruz," HAHR, 77:4 (Nov. 1997), 623. For nineteenth-century travelers' accounts, see Salvador Novo, Breve historia y antología sobre la fiebre amarilla (México: Secretaría de Salubridad y Asistencia, 1964). back
Note 68: Francisco Ajofrín, Diario del viaje que . . . hizo a la América en el siglo XVIII el P. Fray Francisco Ajofrín Capuchino, 2 vols. (Madrid:Archivo Documental Español, 1958), Vol. I, p. 37. back
Note 69: Knaut, pp. 623–4. back
Note 70: James S. Ward, Yellow Fever in Latin America: A Geographical Study (Liverpool: Center for Latin American Studies—University of Liverpool, 1972), p. 18. back
Note 71: Knaut, p. 627. back
Note 72: Ibid., pp. 622, 626–7; on the Spanish American fleet system, see Peter Bakewell, A History of Latin America: Empires and Sequels, 1450–1930 (Oxford: Blackwell Publishers, 1997), pp. 199–200. back
Note 73: Ward, p. 15. back
Note 74: Lourdes Márquez Morfín, Sociedad colonial y enfermedad: Un ensayo de osteopathología diferencial (México: Instituto Nacional de Anthropología e Historia, 1980), pp. 79–81, 99–100. back
Note 75: R. E. Hughes, "Scurvy," in The Cambridge World History of Food, 2 vols., ed. Kenneth F. Kiple and Kriemhild Coneè Ornelas (Cambridge: Cambridge University Press, 2000), Vol. I, pp. 988–9. back
Note 76: Henry R. Wagner Spanish Voyages to the Northwest Coast of America in the Sixteenth Century (San Francisco: California Historical Society, 1929), pp. 245–6, 260. back
Note 77: Margaret Pelling, The Common Lot: Sickness, Medical Occupations and the Urban Poor in Early Modern England (London: Longman, 1998), p. 28. back
Note 78: Gaceta de México, "Engargos,"martes 10 de julio de 1787, Vol. II, no. 38, p. 384; "Engargos," jueves 12 de noviembre de 1795, Vol. III, no. 57, p. 498. back
Note 79: Joaquín García Icazbalceta, Bibliografía mexicana del siglo XVI (México: Fondo de Cultura Economica, 1954), p. 227. back
Note 80: Josefina Muriel, Hospitales de la Nueva España (México: UNAM, 1990), Vol. I, p. 160. back
Note 81: Cárdenas, pp. 221–2. back
Note 82: Aria de Benavides, Secretos de cirugía, p. 66. back
Note 83: Bernal Díaz, p. 262. back
Note 84: Wesley W. Spink, M.D., Infectious Diseases: Prevention and Treatment in the Nineteenth and Twentieth Centuries (Minneapolis: University of Minnesota Press, 1978), pp. 305–6. back
Note 85: J. D. Oriel, The Scars of Venus: A History of Venereology (London: Springer-Verlag, 1994), pp. 35–41. back
Note 86: Crosby, The Columbian Exchange, pp. 124–5; Jon Arrizabalaga, John Henderson, and Roger French, The Great Pox: The French Disease in Renaissance Europe (New Haven, CT: Yale University Press, 1997), pp. 25–6. back
Note 87: Allan M. Brandt, "Sexually Transmitted Diseases," in CEHM, Vol. I, pp. 566–7; Esteyneffer, Vol. I, p. 346. back
Note 88: Crosby, The Columbian Exchange, p. 123. back
Note 89: Oriel, p. 11. back
Note 90: Crosby, The Columbian Exchange, pp. 122–47; Allan M. Brandt, "Sexually Transmitted Diseases," in CEHM, Vol. I, pp. 562–5. back
Note 91: Margaret Pelling, The Common Lot: Sickness, p. 204. back
Note 92: Francisco del Paso y Toncoso, ed., Epistolario de Nueva España, 1505–1818, Vol. XV (México: José Porrúa e Hijos, 1940), p. 59. back
Note 93: Alonoso López de Hinojosos, Suma y recopilación de curugia con un arte para sangrar muy útil y provechosa (México: Academia Nacional de Medicina, 1977). back
Note 94: Ciudad Real, Vol. I, pp. 43, 45–7. back
Note 95: Dones y promesas, pp. 67 (cat. 69), 51 (cat. 104), 57 (cat. 83); Hipólito's ex-voto, 1743: Museo de la Soledad, Oaxaca, Mexico. back
Note 96: "Hernán Ruiz a su mujer Mariana de Montedoca en Sevilla," México: Oct. 21, 1584 in Otte, p. 108–9. back
Note 97: López, pp. 274–6; Esteyneffer, pp. 407–18; "achiote en chocoate" in Ciudad Real, Vol. I, p. 241. back
Note 98: Cecil Textbook of Medicine, pp. 603–8. back
Note 99: Rafael Muñoz Garrido, "Empiricos sanitarios españoles de los siglos XVI y XVII," Cuadernos de historia de la medicina española, Vol. 6, 1967, pp. 101–33, esp. p. 102. back
Note 100: Garcia Icazbalceta, Bibliografía mexicana p. 228. back
Note 101: Ghislaine Lawrence, "Surgery (Traditonal)," in CEHM, Vol. II, p. 979. back
Note 102: AMRT Miravalles, 9 de enero, 1760; RG:V, p. 210; Ciudad Real, Vol. II, p. 18. back
Note 103: López de Hinojosos, p. 104. back
Note 104: Esteyneffer, pp. 235–42. back
Note 105: Gaceta de México, "Engargos," martes 27 de mayor de 1788, Vol. III, no. 9, p. 72. back
Note 106: Ex-voto to Our Lady of Tulantongo. Anonymous, 1774. Collection of María and Gonzalo Méndez, Mexico City, Mexico. back
Note 107: Farfán, pp. 107–13. back
Note 108: AMRT Miravalles, 24 de junio de 1762. back
Note 109: Ex-votos from the Museo de la Soledad, Oaxaca: Joseph Antonio de los Angeles, 10 de junio de 1746; don Francisco Valencia, 26 de enero de 1762; Julian Castellanos, 21 de noveimbre de 1767. back